Optimal Care Pathways for myeloproliferative neoplasms (MPN) patients
- Myeloproliferative neoplasms





Nathalie Cook OAM, who was diagnosed with MPN in 2008, tells the story of the delay in her diagnosis and how after attending a conference in the USA, on the flight home, she made the decision to try to get Pegasys on the Pharmaceutical Benefits Scheme for people with MPN in Australia. It took 7 years to achieve this goal and the hearing her share the story of how she made it happen is truly astounding.

When Debbie McFarlane was diagnosed with the myeloproliferative neoplasm (MPN), polycythaemia vera (PV) in 2013, she didn’t realise it was a form of blood cancer.

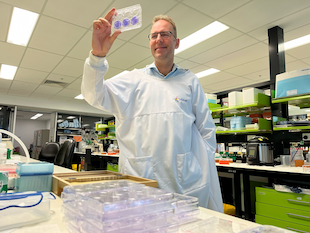
A new monoclonal antibody, discovered by accident by Adelaide researchers, could become the world’s first effective treatment for primary myelofibrosis (MF).
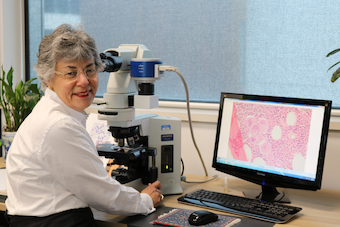
Professor Wendy Erber and her research team in Western Australia are developing a monitoring tool they hope will identify MPN patients who will go on to develop leukaemia.

It’s emerging in all cancers, but particularly in the MPNs, that “genomics is everything” according to Professor Andrew Perkins, an expert in myeloproliferative neoplasms (MPN).
