An antibody for myelofibrosis – “that’s a true discovery”
A new monoclonal antibody, discovered by accident by Adelaide researchers, could become the world’s first effective treatment for primary myelofibrosis (MF).
And if all goes well, early phase clinical trials for the novel therapy could start “within a year”, and scores of people in Australia and overseas have already put up their hands to go on the studies.
The current treatment for MF only controls symptoms and this form of blood cancer can progress quickly over a few years, resulting in severe fibrosis of the bone marrow. In about 20% of people with myelofibrosis, if left unchecked, this severe type of myeloproliferative neoplasm (MPN) can transform to acute leukaemia.
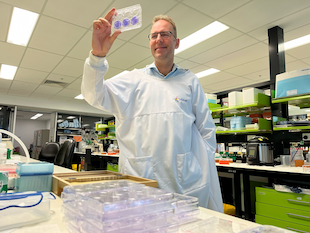
“We still don’t know why some patients progress quickly and some slowly. That’s why I study it,” said Associate Professor Daniel Thomas, a clinical haematologist and pathologist who leads the Myeloid Metabolism Laboratory at the South Australian Health and Medical Research Institute as an Associate Professor of Medicine and was part of the discovery team.
“By understanding myelofibrosis, you have the potential to discover breakthrough treatments for both acute leukaemia and diseases caused by fibrosis.
“The myelofibrosis antibody is a big step forward because it proves that immunotherapy can actually stop the bad cells from dividing. This is significant because myelofibrosis is a rare disease that not many people have done much work on until now, so it continues to be a great unmet need.”
Speaking at the New Directions in Leukaemia Research (NDLR)* meeting in Brisbane (May 30-1 June 2022) Dr Thomas explained the significance of this work so far, which “showed for the first time, ‘proof-of-principle’ using carefully collected patient samples, that you can definitely target myelofibrosis with antibody therapy”.

“We, and other scientists, have wondered if this was possible for a while,” he said. “If you don’t believe that something is possible, then generally nothing changes. Science is funny like that.”
“But no one knew for sure whether the mutant protein that causes the disease actually gets outside the cell and then sends a signal back in, telling it to divide uncontrollably.
“We’re the first to really have strong data that you can block growth of the bad cells (mutant platelet-forming stem cells) that produce the symptoms, and that’s extremely encouraging for patients because we’ve got excellent evidence that it doesn’t hurt normal, good blood stem cells.”
“It really was serendipitous,” said Dr Thomas describing the discovery.
“It was firstly because we were working with some outstanding biochemists (Denis Tvorogov, Frank Stomski) and working in the laboratory of Professor Angel Lopez**, a longstanding mentor and PhD supervisor. Denis and Frank were making molecular tools to further our research by generating new antibodies, but never did we expect the antibody would actually block growth of the disease.
“What this means is that we think we have a surprising double hit here: an antibody likely to be effective in patients, and an antibody that is unique in that it teaches us the how and why the disease arises. So we can now use this new understanding to develop other tools that allow us to predict and protect against the disease,” said Dr Thomas.
“As we were making an antibody to try and understand how calreticulin protein worked inside stem cells, we were completely shocked when we noticed that it actually stopped the cancer cells’ growth.”

Dr Thomas first assumed the results were a mistake, thinking “this is too good to be true”.
“We decided we needed to repeat it, and the results repeated, and we did it in multiple different ways and with other mutations also found in myelofibrosis,” he explained.
“Then we used patient samples that all had calreticulin mutations and that worked as well. Then we went back to normal, healthy stem cells and it did not stop them growing,” said Dr Thomas.
“It’s quite rare to get such a wide therapeutic window of opportunity.”
“I am just so happy our team kept working so hard despite all the setbacks, supply disruptions, and lockdowns during COVID. There are so many critical parts of a good team. Australia needs to re-invest in basic biochemistry as well as encouraging doctors to pursue research,” said Dr Thomas.
Now this monoclonal antibody and a humanised version is being tested in pre-clinical models, “to make sure it’s safe before clinical trial and upscaling”.
“We will only go forward if I’m convinced it’s not toxic, that it works at removing the nasty myelofibrosis cells, and we can mass-produce the antibody without losing effect,” said Dr Thomas.
“That’s called good manufacturing and quality control for biological products, something in which Australia is finally now gaining skills and experience. In some ways, COVID has accelerated the need for Australians to become skilled manufacturers again. Unfortunately, many useful antibody therapies given to cancer patients in Australia are generally made offshore.”
If all that works out, Dr Thomas, Professor Lopez and his team need to raise sufficient funding for a clinical trial.
“Trials are expensive and there are many unexpected costs including the registration paperwork to be given a license to do a first-in-human study, antibody manufacturing, distribution, and careful trial monitoring,” said Dr Thomas who has already been contacted by numerous MF patients from around the world asking if they could go on a clinical trial for this potential treatment.
“That’s unheard of.
“Many of them are under 50 years old and don’t have many [treatment] choices.
“I think this [antibody] or a similar one that was even more potent could definitely control this particular type of myelofibrosis and it would have a high chance of slowing down the disease and improving symptoms.
“We know it works on patients with calreticulin (CALR) – the second most common mutation that causes myelofibrosis.”
“CALR is a causative mutation that drives the disease, it drives the fibrosis, the big spleen and makes people feel fatigued, anaemic, and gives them fevers. Many symptoms of myelofibrosis are surprisingly similar to long COVID,” said Dr Thomas.
“What’s exciting is that our antibody works directly against the mutant protein that’s encoded by the CALR mutation by binding to it and pushing it off the surface of the cell so it can no longer signal,” said Dr Thomas.
According to the abstract in the article, Targeting human CALR-mutated MPN progenitors with a neoepitope-directed monoclonal antibody, published in the scientific journal, EMBO Reports, in February 2022, this research data demonstrated a novel therapeutic approach to target “a problematic disease driven by a recurrent somatic mutation normally considered undruggable”.
Dr Thomas said the media release for this article generated more than 20 million hits worldwide, “underscoring the unmet need for patients and their families”.
“I don’t know whether it will reverse their fibrosis, but we can also take the binding portion of the antibody and turn that into a CAR T-cell that could have curative potential,” he said.
“And it gives hope to other patients with lots of other blood cancers and solid tumours where we can find similar tags – these little neoepitopes that occur and that are not normally found on normal cells.
“And it does raise the possibility that antibody therapies could also be used for the other MPNs – polycythaemia (rubra) vera (PV) and essential thrombocythaemia (ET),” said Dr Thomas who is already doing a trial with an antibody therapy (an Australian invention) for another rare disease, CMML.
Progressing to clinical studies
Dr Thomas is designing the clinical trial protocol and 12 patients will be involved in the initial dose escalation phase trial in South Australia.
“If they all did well, without toxicity, we would expand the trial to Phase II. There’s no control arm in early phase trials – we’re just looking for a response which we measure carefully with molecular studies and spleen size,” he explained.
“Details will be available on the Australia New Zealand Clinical Trials Registry website once the study is approved.
“We would likely have early results within six months of the trial starting because we expect a number of patients who could be recruited quickly, and we would know within about eight weeks whether their CALR mutant cells had gone down or up and if their spleen went up or down.”
In the meantime, Dr Thomas is developing new classes of therapies for patients with JAK2 positive disease.
“This type of myelofibrosis is probably not going to respond to an antibody, but there are some exciting new drugs in development. The structure of the part of JAK2 that causes the disease has finally been revealed and it really gives us some hope for these other patients as well.”
People with CALR positive myelofibrosis who are interested in the potential MF clinical trial are encouraged to email Dr Thomas directly on: haematology[email protected]
Medical or science students who want to learn more about building new types of cancer therapy can contact Dr Thomas: [email protected]
* Assoc. Prof. Thomas said, “top scientists and doctors throughout Australia, as well as international guests come together at NDLR to solve problems and come up with better therapies for blood cancers. We urgently need to reinvigorate medical science for young Australian researchers after the disruptions of COVID and this meeting was a proven example of this”. NDLR is held every two years and has been supported by the Leukaemia Foundation since the first meeting in 2006.
** Professor Lopez served for many years on the Scientific Advisory Board of the Leukaemia Foundation.
Last updated on July 29th, 2022
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.