Latest PBAC outcomes
The latest myeloma drugs to be considered by the Pharmaceutical Benefits Advisory Committee–elotuzumab (Empliciti®) and ixazomib (Ninlaro®)–were not recommended for listing on the Pharmaceutical Benefits Scheme (PBS).
Submissions for both drugs went before the November 2020 meeting of the PBAC which made a first time decision not to recommend elotuzumab in combination with lenalidomide and dexamethasone (ELd) for relapsed and refractory myeloma or ixazomib in combination with lenalidomide and dexamethasone (ILd) for relapsed and refractory myeloma.
“To understand the safety profile and patient experience of this therapy, a Melbourne-based clinician who specialises in myeloma was consulted,” said Ms Forrest.
The clinician had treated several patients with elotuzumab in combination with lenalidomide and dexamethasone in the context of a third line therapy for relapsed or refractory myeloma.
The clinician noted that elotuzumab combination infusions were much better tolerated than carfilzomib and had fewer side effects, and infusions were just as well tolerated as the anti-CD38 antibodies daratumumab (now approved by PBAC) and isatuximab (currently undergoing clinical trials). Also, that this combination therapy extended the life of two of the clinician’s patients by approximately a year, and of another by 18 months.
Given how well patients tolerated this therapy, its clinical benefits (fewer side effects, fewer hospital visits and ease of administration by the clinician) when compared to comparators like carfilzomib, coupled with evidence of overall survival benefit, the Leukaemia Foundation’s submission urged the PBAC to recommend this treatment for listing on the PBS for eligible patients.
Comments were also sought in relation to Takeda’s submission for ixazomib in combination with lenalidomide and dexamethasone for patients with relapsed or refractory multiple myeloma. The Leukaemia Foundation spoke to two myeloma patients from regional Victoria who had been treated with ixazomib in combination with lenalidomide and dexamethasone.
One patient, who had accessed ixazomib for nearly two years through a compassionate access scheme, stated that the ease and convenience of a weekly tablet was important to them, and was much less intrusive to their life than needing to travel some distance to a treatment centre for infusions:
“It was so easy to take. One at the beginning of the week. Very convenient and easy. I feel it helped me. Living in the country it was so much easier. It was fantastic. What it meant for us, because I’m 72, is I’m still alive. Life is lovely and I am very blessed. Living in the country it made it so much easier that having to go to a larger centre for infusions. At the beginning of my treatment I was going to have infusions. It was quite a drive. This was so much less intrusive into life. I felt so grateful actually.”
This patient said the treatment started working quickly. Due to some side effects this patient stopped the treatment and still had negligible levels of disease at the time of the interview.
The second patient echoed these sentiments, saying the oral dosing regimen was easy to understand and more convenient than infusions. They remained on the treatment and had not had any side effects.
The Leukaemia Foundation spoke to a Sydney-based clinician who had treated relapsed myeloma patients with the ixazomib combination regimen who had expressed a preference for oral regimens as it reduces the requirement to attend hospitals or treatment centres considerably, and also spares them repeated injections/cannulations for infusions. The clinician stated that these patients had found the dosing regimen easy to grasp.
The clinician also highlighted the considerable progression free survival in patients who have high risk cytogenetics (TOURMALINE study), and being in a group with few good options, the ixazomib combination therapy was particularly valuable.
The Leukaemia Foundation also spoke to a Brisbane-based clinician who agreed that in general patients prefer oral therapy – “less hospital visits, who likes needles being stuck into them” – and their patients had found the dosing regimen manageable and preferred administration by injection.
“Given the considerable benefit to patients in time and quality of experience, particularly for regionally-based patients, and where treatment can be as safely and effectively delivered through oral medications as through infusions, enabling access to the oral medication should be a priority for the PBAC, and the Leukaemia Foundation strongly supports a positive recommendation to list on the PBS,” said Ms Forrest.
In December 2020, the PBAC announced its recommendation not to list elotuzumab as it considered that, due to the nature of the indirect treatment comparison (ITC) and differences between the key trials, the results of the ITC were difficult to interpret and did not adequately demonstrate non-inferiority between ELd and the nominated comparator, carfilzomib plus dexamethasone, in terms of efficacy or safety. The PBAC therefore considered that the presentation of a cost minimisation analysis was not appropriate.
The PBAC also did not recommend ILd due to the nature of the naïve ITC and differences between the key trials, the results of the naïve ITC were difficult to interpret and did not adequately demonstrate non-inferiority between ILd and the nominated comparator, carfilzomib plus dexamethasone, in terms of efficacy or safety. The PBAC therefore considered that the presentation of a cost minimisation analysis was not appropriate.
The pharmaceutical sponsor of ixazomib, Takeda Australia, has made a public statement in relation to the PBAC’s recommendation, thanking patients, clinicians and organisations that took the time to provide their experience. Takeda has also stated that the company will continue to work with the Department of Health and the PBAC so that Australian patients may soon access ixazomib through the PBS.
Comments on elotuzumab and ixazomib by Professor Miles Prince
“Both are great drugs,” said Prof. Miles Prince.
“It’s a question of… is their instrumental benefit better than what we already have?
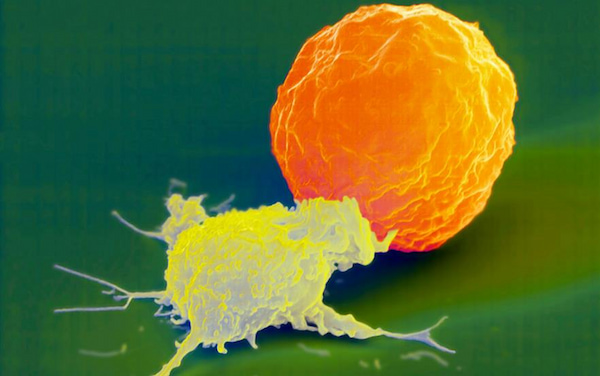
“Elotuzumab is a monoclonal antibody against a protein on the surface of the cell called SLAMF-7.
“The results of the relapse/refractory studies were relatively modest.
“Its place in the relapse setting is limited because all the trials with elotuzumab were before the days of daratumumab, so most patients suitable for elotuzumab in the trials, would not have had daratumumab.
“If it’s going to find a place, it’s got to be early on, perhaps in the first line. There are studies of first-line elotuzumab in older patients, so we may see it make a resurgence.
“I think it would be very challenging to have it approved by the PBAC.
“Although elotuzumab and daratumumab haven’t been compared head-to-head, studies suggest that daratumumab is more potent.
“Ixazomib is an old proteasome inhibitor used in maintenance treatment.
“Current maintenance treatment is lenalidomide, so the question is, could it replace lenalidomide?
“Because there’s no randomised study, it will be challenging for the PBAC to demonstrate that it’s more efficacious than the already approved drug, lenalidomide.”
Last updated on June 8th, 2022
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.