Feeling tired all the time because of cancer
Discover how cancer fatigue impacts daily life and learn ways to manage feeling tired all the time due to cancer. Explore Neda's inspiring story.
- chemotherapy
- Myeloma
- Treatments and side-effects

Discover how cancer fatigue impacts daily life and learn ways to manage feeling tired all the time due to cancer. Explore Neda's inspiring story.

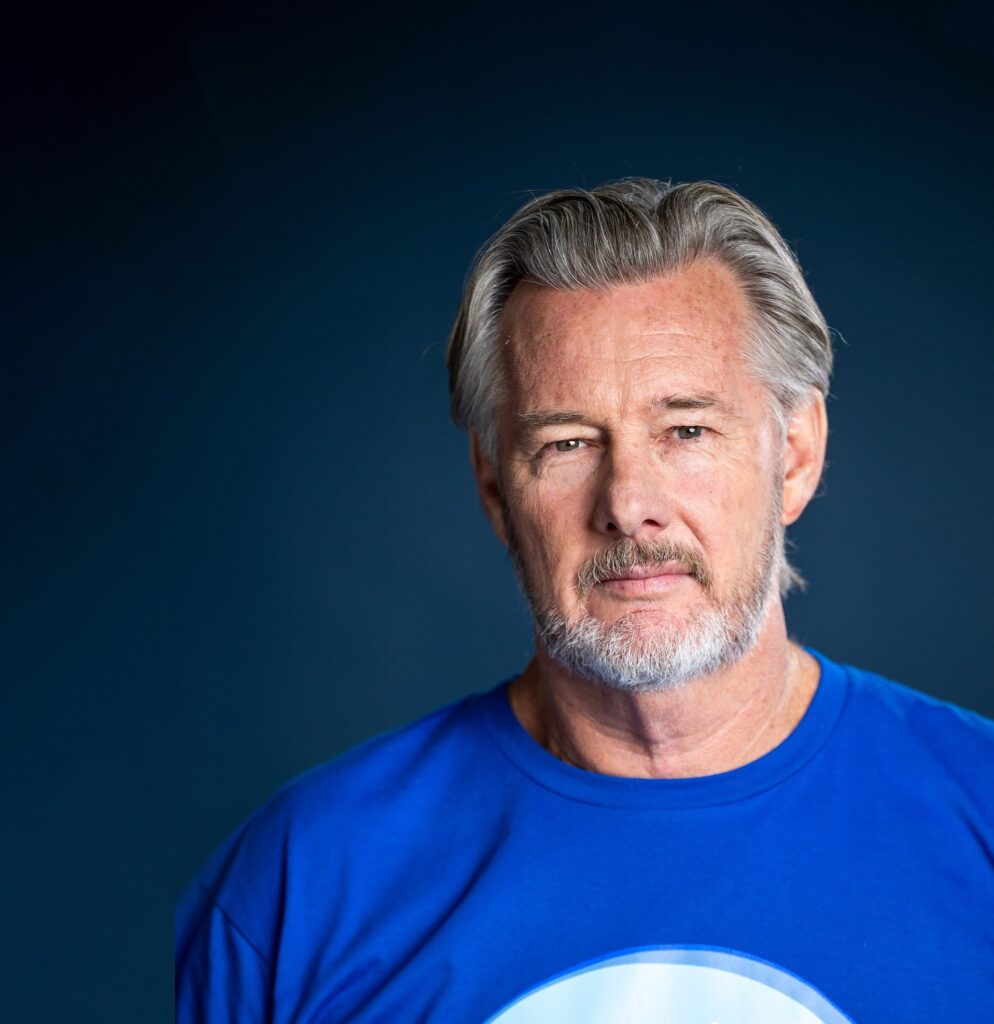
Wayne Douglas spent more than half a lifetime working with heavy rock and concrete in the civil construction industry. In 2018, Wayne joined the roughly 2,600 people diagnosed with myeloma in Australia each year.



Barry Du Bois has today shaved off his locks in a nod to his own journey with the blood cancer myeloma, for the Leukaemia Foundation’s iconic World’s Greatest Shave. It’s no secret that this much-loved and well-known Aussie, has been living with the incurable blood cancer since he was diagnosed in 2017.
Patients understand that clinical best practice care begins with an accurate and timely diagnosis.

Jennifer Marx shares insight into being diagnosed with myeloma at almost 27 years old - a condition far more prevalent in older people. Jennifer shares how she navigated the healthcare system, managed treatment and relationships, and her experience having two autologous transplants.

For the third time, selinexor (Xpovio®) will be considered by the Pharmaceutical Benefits Advisory Committee (PBAC) at its November 2022 meeting for the treatment of relapsed/refractory (R/R) myeloma.
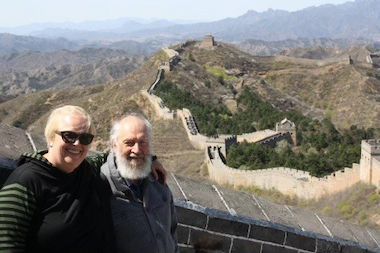
During the 22 years Martin Boling has had myeloma, blood cancer of various types has affected four other members of his family too, not just him.
Meet the research team developing a myeloma treatment with maximum efficacy and minimal side effects
