Optimal Care Pathways for leukaemia patients
- Acute lymphoblastic leukaemia
- Acute myeloid leukaemia
- Chronic lymphocytic leukaemia
- Chronic myeloid leukaemia



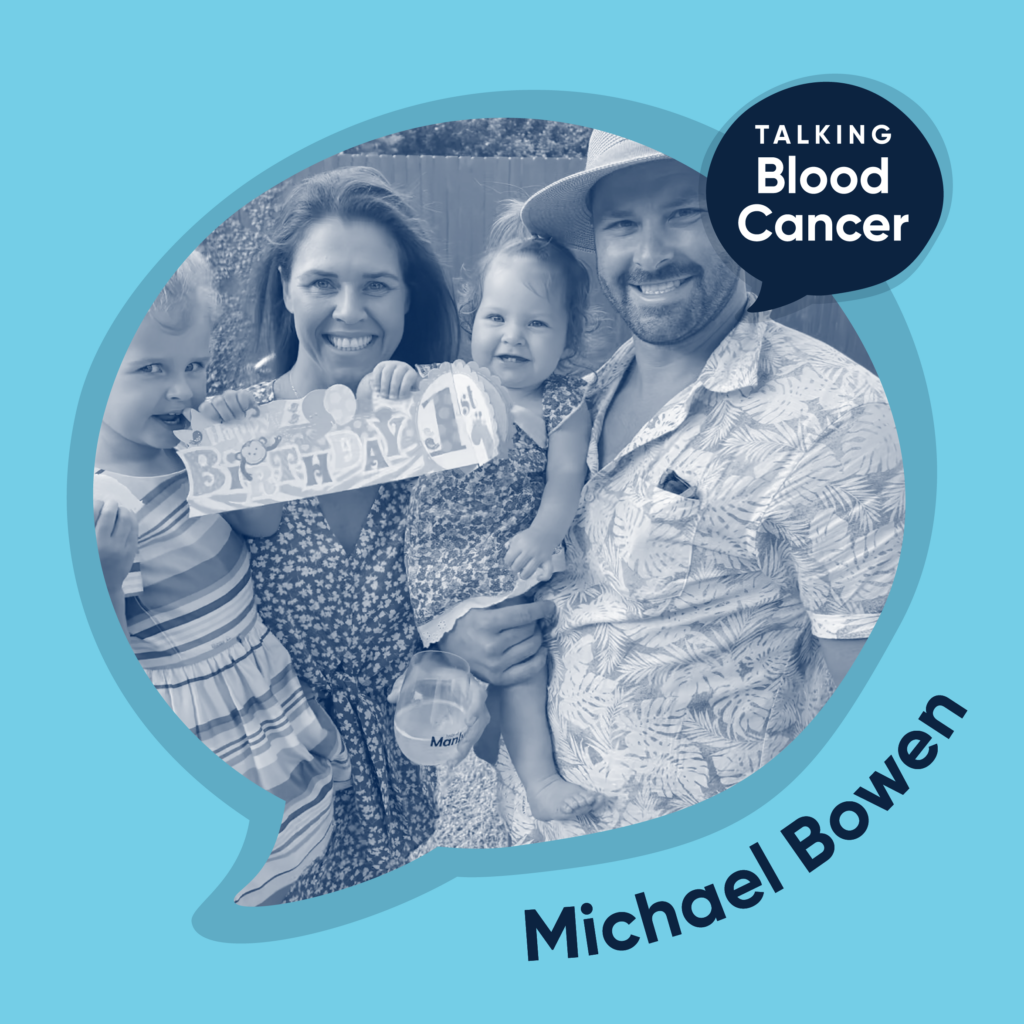
Michael Bowen was 33 years old and living in Sydney when one morning, as he was driving to work, he received a phone call that would stop his fast paced life in its tracks. Michael received a diagnosis of chronic myeloid leukaemia (CML). In this conversation, Michael talks about the bouts of depression he came up against and how he was able to overcome these hard times.
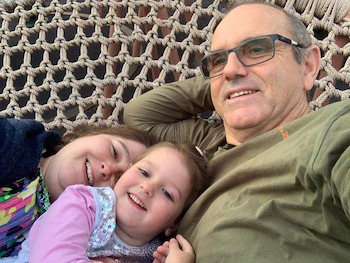
Terry Robson-Petch has been living with CML for 20 years.
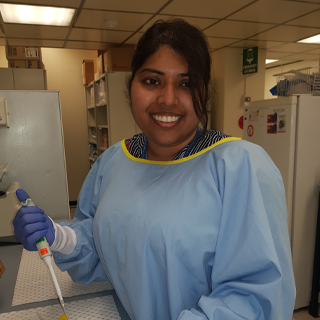
The greatest unmet need in CML is the ability to predict outcomes at the time of diagnosis according to Dr Naranie Shanmuganathan, a consultant haematologist at Royal Adelaide Hospital and SA Pathology.
Dr Pagani has a vision for a personalised approach to treatment-free remission in CML
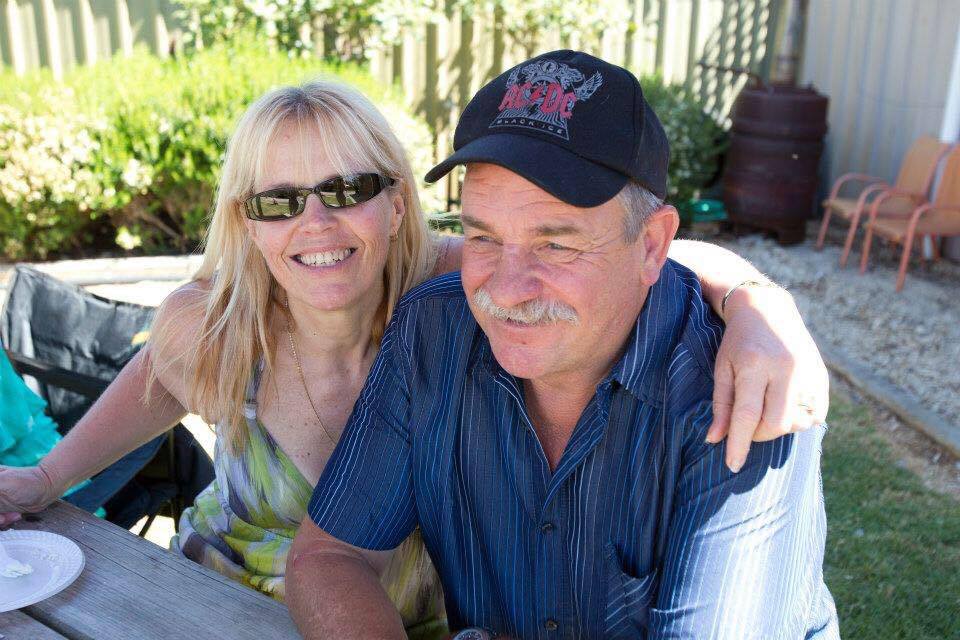
Heather Jenkins was one of the first Australians to go on a clinical trial for the first targeted therapy for chronic myeloid leukaemia (CML).

Newly revised optimal care pathways (OCPs) provide best practice information for the treatment and care of people living with acute myeloid leukaemia (AML), and diffuse large B-cell lymphoma (DLBCL) and Hodgkin lymphoma (HL).

Diagnosed with two blood cancers, Nick's world changed instantly. Then transplant complications challenged him in ways he didn't expect.

Leanne Pitman tells us the story of her 'scary' decision to stop her CML treatment.