Leukaemia Foundation invests $2.8m in innovative lymphoma research
Better understanding and treatment of lymphoma is the focus of eight new research projects that are part of the Leukaemia Foundation’s National Research Program over 2019-2022.
This $2.82 million investment into lymphoma research at some of Australia’s leading research centres is aimed at better understanding the biology of lymphoma, using genomics to inform prognosis and therapy decisions, preventing and treating infection, and includes a genomics and other trials to improve outcomes.
Strategic Ecosystem Research Partnerships (SERP)
Of the Leukaemia Foundation’s nine current Strategic Ecosystem Research Partnership projects, two are focused on lymphoma.
Follicular lymphoma (FL) is the most common subtype of slow growing (indolent) lymphomas, making up 20-30% of non-Hodgkin lymphomas. Professor Maher Gandhi, at the Mater Research Institute (Brisbane), is Establishing a new prognostic score for follicular lymphoma to rationalise therapeutic decision-making and improve patient outcomes. There are two stages of FL – early stage, which is potentially curable, and advanced stage, which is incurable and where current therapy is designed to control symptoms and disease burden. There is no way to predict if a person will respond to treatment or not. The aim of this project is to develop a combined immuno-clinical-genetic prognostic score to help predict which patients are high-risk and may benefit from more aggressive treatment, and which patients are at lower risk and whose treatment can be scaled back to minimise drug-related toxic side-effects. Read more about this project which runs until January 2021.
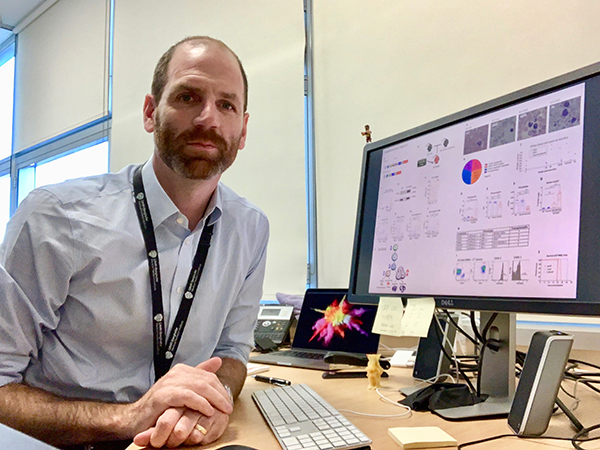

The second lymphoma SERP project is a new blood cancer genomics clinical trial which will be headed by Professor Steven Lane at the Queensland Institute of Medical Research (Brisbane) and Professor Hamish Scott, University of South Australia, SA Genomics (Adelaide). Many patients with high-risk blood cancers relapse or fail to respond to therapy, and the outcomes for these patients are poor. The Blood Cancer Genomics Clinical Trial is a precision medicine pilot study using genomic screening to identify mutations in the cancer cell DNA; allowing for genetically directed targeted therapy for these high-risk patients who have failed therapy. This trial is in the final stages of development and is expected to start recruiting late-2020/early-2021.
Translational Research Program (TRP)
The Translational Research Program is an initiative that aims to take new and innovative research out of the research laboratory and helps move it into the clinic. The Leukaemia Foundation has partnered with the Leukemia & Lymphoma Society (U.S.) and Snowdome Foundation to co-fund these grants. One of the five current TRP projects is for lymphoma, which is the most commonly diagnosed blood cancer in Australia.

The title of Professor Ricky Johnstone’s research at the Peter MacCallum Cancer Centre (Melbourne) is Targeting deregulated epigenetic mechanisms in B-cell lymphomas. One-third of all patients newly diagnosed with non-Hodgkin lymphoma has a diffuse large B-cell lymphoma (DLBCL). As conventional chemo-immunotherapy has a poor outcome for 40% of these patients who either do not respond to the treatment or relapse, there is an urgent need to better understand the biology of DLBCL. Greater knowledge would help to define new clinical biomarkers, design personalised therapies and improve clinical outcomes for these patients. DLBCL is characterised by profound alterations in the epigenome; a group of chemical modifications in the DNA and histones that regulate gene expression independently of the DNA sequence. Between now and the end of Prof. Johnstone’s three-year research project, in July 2022, his lab is examining agents that target this alteration of the epigenome, to determine if pre-treatment sensitises DLBCB cells to subsequent chemotherapy. The institutions that are collaborating on this project are Monash University (Melbourne), and in the United States, Weill Cornell Medicine (New York), University of Miami (Florida) and Jackson Laboratory Cancer Centre (Maine). Read more about the search for biomarkers and better treatments for B-cell lymphomas.
PhD scholarships
The Leukaemia Foundation is helping the brightest medical and science graduates pursue a research career in blood cancer by collaborating with the Haematology Society of Australia and New Zealand (HSANZ) to co-fund PhD scholarships.
Over the last two years we have been proud to award six scholarships through our PhD Scholarship Program and five of them involve lymphoma.

Dr Wei Jiang, of the Westmead Cellular Therapies Group (Sydney), is one of our current PhD Scholarship recipients. Through her project, Clinical safety and efficacy of T-cell immunotherapies for infection and malignancy, Dr Jiang will participate in two clinical trials which could have a significant clinical benefit for patients who take part. One of the trials involves harnessing the power of a new type of engineered immune cell, called CAR-T (chimeric antigen receptor T-cells) and the other trial is looking at the use of pathogen-specific ‘smart’ T-cells in the treatment of resistant viral infections in patients who have had stem cell transplants.

At the Walter and Eliza Hall Institute of Medical Research (Melbourne), Elizabeth Lieschke is investigating the mechanism by which tumour suppressor gene, p53, prevents the development of leukaemia, lymphoma and other cancers; and the processes by which activation of p53 kills malignant cells. The aim of this study is to understand why some blood cancer cells die, while other cancer cells undergo cell cycle arrest/cell senescence and therefore are more likely to relapse following cancer therapy. Ms Lieschke and her team hope to identify biomarkers that will help predict the nature of the response of cancer cells to drugs that activate p53, leading to therapies that will be more personalised and targeted. Mutations in p53 occur frequently in blood cancers that relapse following therapy and for these patients the prognosis is extremely poor. A deeper understanding of the impact of mutations in p53 will inform the design of new therapies that are desperately needed to improve the prognosis for these blood cancer patients. They could act downstream of p53 and efficiently kill mutant p53-expressing blood cancers. Read more about unlocking the key to understanding cell death.

Dr Khai Li Chai of Monash University (Melbourne) is one of our current PhD Scholarship recipients. Her project title is Immunoglobulin therapy to prevent and treat infections in patients with blood cancers: who, why, when and how? Patients with non-Hodgkin lymphoma and other blood cancers who have had an allogeneic stem cell transplant frequently develop a condition called hypogammaglobulinaemia due to their disease or its treatment. In people with this condition, the body doesn’t produce enough antibodies which can result in serious and/or recurrent infection. It is a significant cause of mortality or morbidity in these patients. Immunoglobulin replacement therapy is often administered to these patients but there are substantial variations in recommendations and practise internationally, and there is no clearly defined standard of care. This project will evaluate current practise and clinical outcomes of immunoglobulin treatment and investigate how detailed patient immune profiles can be used to guide and monitor optimal dosing and duration of immunoglobulin therapy.

Julian Lindsay is a bone marrow transplant pharmacist and his research project, Antifungal management optimisation in haematological malignancy and haematopoietic stem cell transplantation, is aimed at preventing infections in people with blood cancer and those undergoing bone marrow transplants. These patients have highly suppressed immune systems due to having chemotherapy and the transplantation techniques used to achieve better cure rates. Based at the Fred Hutchinson Cancer Research Center in Seattle (U.S.), Julian will address critical knowledge gaps related to specific patient risk factors for developing infections such as cytomegalovirus, Epstein-Barr virus and invasive fungal infections, and investigate the optimisation of antimicrobial therapies to prevent infections and improve the survival of these patients.

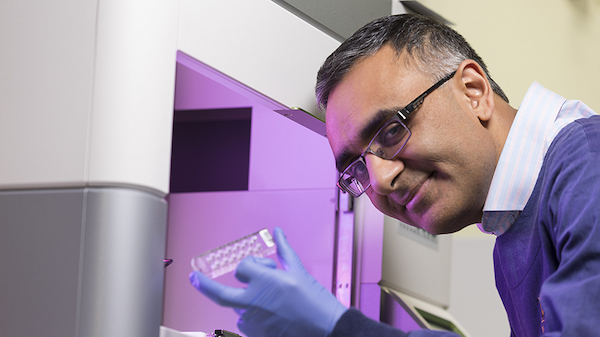
Dr Karthik Nath is a haematologist undertaking his PhD at the Mater Research Institute (Brisbane). His research seeks to develop a deeper understanding of the biology of follicular lymphoma (FL) and to use this to predict an individual’s response to treatment using evolving genetic and molecular laboratory technologies. Dr Nath plans to incorporate these elements at the point of diagnosis in FL as a practical way to improve diagnostic techniques and treatment approaches with real-world applicability. The second part of this research titled, Integrating immunity and genetics into follicular lymphoma to establish a prognostic score fit for the modern era will use precision medicine to treat patients with FL by applying patient-specific immunological, molecular and genetic markers in prognostication. The aim being to improve patient outcomes through individualised treatment approaches. Read more about better understanding and improving treatments for FL.
Last updated on February 18th, 2022
Developed by the Leukaemia Foundation in consultation with people living with a blood cancer, Leukaemia Foundation support staff, haematology nursing staff and/or Australian clinical haematologists. This content is provided for information purposes only and we urge you to always seek advice from a registered health care professional for diagnosis, treatment and answers to your medical questions, including the suitability of a particular therapy, service, product or treatment in your circumstances. The Leukaemia Foundation shall not bear any liability for any person relying on the materials contained on this website.