A trial put Joe in remission for six years and counting
Joe participated ina trial which he says saved his life.
- Amyloidosis
- Clinical trials
Joe participated ina trial which he says saved his life.
An amyloidosis clinical trial described as “a staggering result, almost never seen in blood cancers”.

Expert interview series: Associate Professor Peter Mollee discusses issues around AL amyloidosis

Fahimeh had an early amyloidosis diagnosis.

Jack was 22 years old when he was diagnosed with a dangerous blood disorder called aplastic anaemia.

Gavin thought leukaemia was only a children’s cancer until the day his shock diagnosis completely changed his family forever.

After relapse last year, Siobhan knew her Leukaemia Foundation family would be there for her again.

Jenny connected with the vital information she needed to find her best treatment and take on her blood cancer with confidence.

Generous support helped deliver a research breakthrough that could lead to the first drug approved for patients with AL amyloidosis.

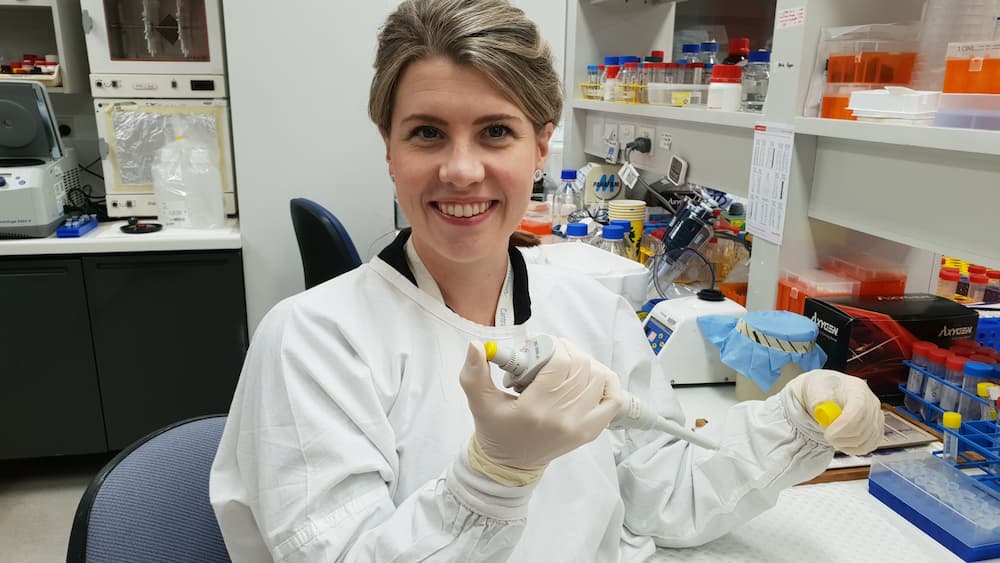
Dr Liesl Butler is just one of the promising young blood cancer researchers boosted by kind supporters.