Blood Wars: My body’s rebellion
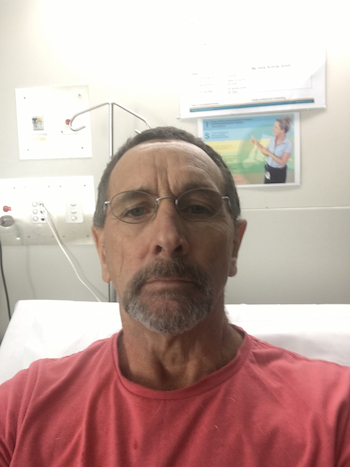
Since his initial diagnosis with blood cancer in 2017, Tony Wakely has written about his experiences with MDS and AML in a journal on his computer, cataloguing what he’s been through, his thoughts and emotions.
“It was a way of stress relief,” said Tony, who has chosen to share this detailed journey with you.
The following personal account is by Tony Wakely.
Beginnings 2017
It started as just another Friday, May the 12th 2107. Who knew what was about happen and how life-changing it would be.
I started the day as usual for a day shift week, up at 4.30, breakfast and off to work with my wife Karen. All good so far. Started my shift ok and all was going well. My partner in crime for the day, PJ, and I were going about our work quite nicely and everything seemed to be ok, until I had to go and see another operator about an issue he was having. After climbing two flights of steps, twice, and returning to my workstation, I knew something wasn’t right.

Great that’s all I needed to hear, but at 57 I thought, would not have been unusual, but he then said he wanted to do some blood tests just to check some things out and then he, in consultation with my normal GP suggested I take some time of work to rest and to come back and get the blood test results on Tuesday morning.
So, off I trundle to the doctors on the Tuesday to get my blood test results and to me and my doctors surprise, I’ve got anaemia… with a twist. I also have high iron as well, which at the time of knowing bugger all about blood, was an impossibility.
He had been so confused by the abnormality of the blood results, that he immediately sent them to the haematology department at the Princess Alexandra Hospital in Brisbane to see if they could make some sense of what was going on with my blood counts.
In the meantime, he was and in consultation with my usual GP, they were treating this as the possibility of a TIA, so they decided to run more tests to eliminate this as a possibility. So it was off for more blood tests and it was also suggested that I have an MRI on my head just to ensure there was no neurological issues going on.
During this time I also had my two sisters coming over from New Zealand for two weeks and also my brother was coming up from NSW. Great time to have visitors, just when I’m feeling not on top of the world.
But I managed to get through the period ok and it was a good distraction from what was going on, and at the time I never told them of the issues I was having as I did not want to ruin their holiday. But on the night before they were due to leave, I came clean.
As I said, I had to have an MRI, so I duly went along with Karen in tow to have my MRI, to see if the three brain cells were still in place and functioning ok.
Test results showed that I had not had a stroke or that there was any sign of tumour, which came as a relief on some points, but still concerned me as to what the issue could be.
During this period other tests were carried out on my kidneys, heart and lungs trying to eliminate all the usual suspects from their enquiries, but still my blood counts continued their plunge down the scales. My platelets dropped to 85 according one my latest blood tests … I remember thinking at the time. What the hell are platelets? Over the course of the next six months I would learn what they were and a whole lot of things that I thought I would never think I would ever learn. The whole issue of having anaemia is that the cure for it is to give you iron. Not possible for me, I had high iron already. It also created problems with fatigue and shortness of breath as well, which was great as I was already an asthmatic. I had great support at work, not only from my team mates but my company as well during what was a very trying time both physically and mentally too.
Diagnosis at the PA
On June the 20th I had my first hospital appointment at the oncology day care ward at the PA (Princess Alexandra Hospital) where I meet a lovely young haematology registrar named Mimi. She asked me a few questions about symptoms, etc., reviewed my latest blood tests and, in consultation with the head haematologist, came to the conclusion I had a form of leukaemia called myelodysplastic syndrome (MDS).
I think I sat there like a stunned mullet thinking the diagnosis was wrong. But then it was explained to me that this form of leukaemia was due to misfiring bone marrow and that at the moment it was just a case of keeping an eye on it with blood tests every 12 weeks to see how it was progressing and then formulate a plan of attack if required. I was also told that this thing could sit in my body for the rest of my life and never cause me any issues, but I’m not that bloody lucky.
More blood tests were asked for and once more I gave more vials of blood. I was starting to feel like a bloody pin cushion by now. I was informed that if anything changed in the interim then they would be in contact with me. Otherwise they would see me in 12 weeks.
Things did change apparently. Less than a week later I got a call informing me that my blood work was again full of inconsistencies and that my 12 week appointment had now been changed to 6 weeks’ time and a letter with a new date and time would be sent out.
At this time, it was suggested that I cut out all forms of alcohol. I thought what the hell is this all about, but it had a lot to do my kidney and liver functions, which they thought at the time was being affected by my alcohol consumption, so that weekend I finished off the last 6 pack in the fridge, much to Karen’s protests at the time. I have remained sober since the first weekend of July 2017.
So the new appointment time turned up and it was for August the 8th, for another consultation, this time with another registrar, Kate, who informed me that things were changing quicker than they had first thought they would and my blood counts were still dropping, but not enough to warrant performing a bone marrow biopsy at this stage, but she would consult with head of haematology just to see what was going to be the next step.
After about 10 mins Kate returned and informed me although my blood work did not fall in the criteria for a bone marrow biopsy, they were going to do one anyway just to try and figure out what was going on, and made an appointment to return on the Friday to perform the biopsy.
So once again Karen and I head off to the PA for more tests. This time they were going to sedate me and take a small sample of bone marrow for my hip and a piece of bone, then they would test it for any abnormalities. I was told they would contact me in the next few days with results and then we would know exactly what was going on.
Again, with the nature of everything that had been going on with me, the call came at 4pm that very afternoon and all Kate said was that things were a little more serious than they had first thought and that an appointment had been set up for me on Tuesday the 15th of August at the oncology ward at the PA. On the Monday I informed my manager that things were changing quickly for me and I had an appointment at the hospital on Tuesday and that I would probably be late for work on Tuesday. He was ok with that. In fact, work had been pretty good with the whole affair up until this stage.
D-Day August 15 2017
We arrived for my appointment once again at the PA, to at last get hopefully some answers. At first we met with yet another registrar, Matt, and he said we would be joined by one of the more senior haematologists soon. So I thought, well this can’t be good, and after about 5 minutes of checking on how I felt, etc., in walked Sally Mapp, and she quietly informed me that I had leukaemia… a particularly nasty form called acute myeloid leukaemia (AML) and that on Thursday 17th I would be admitted to the oncology ward 2E, for a month, to start an intensive round of chemotherapy, called a 7/3 induction chemo.
It seemed to me at the time, that time stood still. I’m going holy shit I have cancer and I’m being given 2 days’ notice that I’m going to start an intensive round of chemo. Once the initial shock passed and I was able to process what had just happened, I then asked what it all entailed, risks and outcomes, etc.
I was told that although the induction chemo was a tough regimen over a 7-day period, where I was plugged into a chemo drug called cytarabine for those 7 days, and another drug, idarubicin, was given to me for the first 3 days as a quick transfusion over a 30-minute time frame.
Also, I was given a list of the side effects from chemo, ie: nausea, headaches, fever, hair loss, and all sorts of other nasties, but at the end she said I could die from the chemo as well. It sounded like a list for the 7 plagues of Egypt. But this was rare, only 5% of patients experience this, and they have to be really ill for this to occur.
She said I was lucky, didn’t feel it to me, that I had been caught in the early stages of the disease so my recovery should be up in the 95% success area. But there were still risks involved, doing nothing was not an option, so it began.
We spent the rest of the next hour going through everything I needed to know concerning my illness and what a lot of the terms I was going to hear during my treatment meant, and whatever else was going to crop along the way. So, I was told to rock up to ward 2E at 9.30am on Thursday to be admitted into hospital.
We then had an intensive conversation with one of the cancer support nurses from 2E, Camilla, who outlined what services would be available me during my stay and, some of the support services also available to Karen as well.
So far, the day had just been a whirlwind of information, a lot of it scary, but all the people we dealt with were amazingly supportive and it was reassuring that I was going to be in good hands. At the end of the day, I came to the conclusion that I could not change what had happened and that to win this battle I would need to remain as positive as I could throughout the entire process. As I pointed out to people later on, it was never the diagnosis that frightened me, it was all the bloody toxic crap they were going to pump into my body that scared the hell out of me.
We both came to the conclusion, as we left the PA at 3.30pm, having been a long day, that we were not going back to work, as we had so much to digest, and plans to put in place. So, I rang my manager, informed him that I would not be in, which they suspected was going to be the case, and that I would like a meeting with him and Karen’s manager at 10.30am the following morning. We also spent the evening ringing family members to inform them of what I had and what lay ahead for me. Not a lot of joy in making those calls but it needed to be done.
So off we went to the next day, following a fairly restless night, to our meeting at work and in we went to the appointed room. Our mangers were both there and looked at Karen and I with querying eyes, especially in the light of our no show the day before, and I just came out and said that I had been diagnosed with leukaemia and I was heading into hospital the following day, for a month, to start chemotherapy.
There was a silence like nothing I’d ever experienced before. I think the two of them were more shocked than I had been the previous day. Anyway, I got down to explaining what was going to happen and that I would probably be off work for a period of time, of which I had no idea on how long, and I guess we would just see how long that played out. But more importantly, Karen was also going to require time off at odd times, for appointments I had to attend, etc.
I must say that they were extremely helpful throughout this entire process and once we had sorted that out I then headed over to HR to sort out some of the other stuff as well. Our HR manager has a bit of a reputation for being a bit of a hard nut, but when I explained all that was going on, she could not have been more helpful, set up all the things I needed to apply for for my income protection application, ensured I was still paid up until that kicked in, etc. So I left work feeling in a much better mood knowing that all those bases had been covered.
Next we went to the bank to see how they could help, but although we made some minor changes to how things worked, they really weren’t that helpful. All in all, an extremely busy 24 hours ….. I was happy just to sit down and a have a quiet coffee at the end of the day.
Hospital and treatment
We arrived at the pre-determined time at the hospital, only to be told that I was not expected at that time, but after an hour of waiting I was finally admitted into a four-bed room. It seems there was a hive of activity around my arrival with nurses popping in to check my vitals, temperature, heart rate, pulse and breathing, which I was to learn very quickly, was going to be done every 4 hours during the day and night. I had an early visit from a specialist who quizzed me on a few things regarding my diagnosis and also about my hepatitis. It seems I would have to start a suppressant drug for my hepatitis, so it did not interfere my treatment and all the other pills I was taking were also changed to what brands were required so nothing would hinder how the chemo drugs worked.
I had a number of tests scheduled for the next 2 days as they could not start chemo until things like lung function and heart tests were performed. These were to ensure my body could handle the stresses that was about to put on me by treatment. So, more prodding and poking by the medical profession, but at least we were starting to get somewhere.
On the Thursday afternoon, I had a central line inserted in my left arm, into one the major arteries that went back to the heart. In fact, it runs to within 5mm of the heart itself. So not only are they going to try and poison me, but they are going to put it straight into my heart. But seriously, it is the best way to get the chemo drugs throughout the body quickly, by using the best pump ever designed. I was now firmly ensconced into the Queensland health system, with my nifty purple gown, my wrist band and my unique UR number, 2049818; sounds like a prisoner’s number or a barcode. I thought how it was rather a long number, and every time any treatment or anything was done, they always asked what your UR number was, name, and date of birth. I asked the nurses why they asked the same questions every time. It was to ensure they had the right patient, and remember I was lying there about 3 weeks into my stay. What did they think?… someone had slipped in and taken my place, so they could have free drugs and hospital food!.
On the food side of things, it was the one side of my stay that surprised me, as past experience had taught me that hospital food was crap. But at the PA, the food was actually quite good with good variety and was not the tasteless horrid stuff of days gone by.
I was moved to a single room on the 18th so I could start my chemo. They keep chemo patients isolated in a single room for two reasons. One, is after a few days of chemo you become cytotoxic from the chemo drugs which means all bed linen, clothes, etc, are all impregnated with the toxins that are excreted out of my pores in sweat, etc, so they are quite dangerous to others. And also, once the chemo drugs start to attack my bone marrow and other parts of my blood, my immune system is left in tatters, which makes me vulnerable to any infection or virus going around.
I finally got to start my chemotherapy treatment on Sunday the 20th, at about 11am. In came two nurses dressed in purple gowns, gloves, and all the trimmings to protect them from any mishaps that may occur whilst setting up the drugs. I’m once again asked name and date of birth, and away we go. Hitch up the chemo, turn the pump on, and away we go. This was my daily routine every day for the next 7 days; come in and change over bags of cytarabine and do the 30-minute infusion of idarubicin.
During all this, I still have my four-hourly obs performed, I had daily visits from all the doctors who are keeping an eye on me and the constant change in nurses. So although I was in a single room, I was rarely alone. Also, Karen was a constant visitor, so it was good to have her there as support too.
I had from day 1, I had my laptop and a hard drive with a whole pile of movies and TV programs on them so I was able to binge watch the entire five seasons of Breaking Bad, as well as catching up on a lot of reading, so I was very rarely ever bored.
Sally Mapp was my first specialist. I had her for the first 2 weeks of my stay, as there was a specialist roster, where they would rotate through a number of hospitals in Brisbane on a 2 to 3 week rotation. But the registrars were a rather constant number and the main registrar I had was a lovely English doctor, Rebecca, and she was always checking up to see how things were going.
It was really quite a good team of doctors and nurses in the oncology ward at the PA, which made the stressful time that patients have a whole lot easier to deal with, and I seemed to be a bit of favourite with the staff, as I was fairly independent, as I was mobile and had very few issues with the side effects of the chemotherapy. I also had a really positive attitude all the way through the process which made things go a little easier. The other part of helping me through this tough time was the good friends from work and other people who put the effort in to come and see how I was getting on, especially PJ and Robbie from the shift I work on. Our friend, Heather, dropped in a couple of times and Karen’s cousin, Karen, came as well. Without the support of family and friends , I would have done it tough mentally.
On about the third day of my chemo treatment, Sally came in and informed me that there was a complication… surprise, surprise… that they had encountered with me. It seems that they do a DNA screen on all patients at the time of the bone marrow biopsy and it was discovered that there had been a chromosome deletion in my DNA, in particular P53, which is the chromosome which prevents the cancer from returning, and that I would require a bone marrow transplant in the very near future, probably before Christmas or else the leukaemia would return within 6 months.
For the second time in 2 weeks I was rocked by bad news and once again I’m sitting there exploring options on what all this meant.
She asked whether I had any siblings, which I did, two sisters and a brother, and I was asked as to whether they would be donors or not. She also explained that there was a possibility they would not be a positive match and then they would have to go to the world bone marrow register to see if there was a donor elsewhere.
So I hit the phone and rang my sisters and brother, explained the situation to them, and they all agreed to be tested to see if they were a viable match. All it was going to take was a simple blood test, performed by the Red Cross and then, in a few weeks’ time, we would have the results. Funny that less than 4 months prior to this, we had all been in Brisbane having a laugh, a few beers and a good time, and now I was asking them to help save my life. It was a humbling experience to know that my family would do this for me.
Anyway, my chemo was still be pumped into me and as the days wore on my blood counts continued to drop, and by day 7, when I finally came off my chemo, they were just about at rock bottom. Karen came to visit me on the day I came off my chemo as it was a sort of celebration that I had come out the other side without issue, or so I thought.
We were both sitting there having a coffee and a bit of a chat, when all of a sudden, I just began shaking uncontrollably. Later, I found out it called a rigour attack, and I was incredibly cold, so we called for more blankets, but nothing would stop the shaking and this went for about 20 to 30 minutes in which time Sally also came in and said that this was bound to happen and that it looked like I had picked up a virus. Once I calmed down, they would take blood cultures from me to see what I had picked up.
They gave me a fast-acting antibiotic and waited. Once I calmed down, the cultures were taken and by 5pm they had concluded that I had picked up E. coli in one the lumens on my picc line, so I was put on a course of intravenous antibiotics and all was fine. It appears that we carry all these various bugs in our system all the time, but they are kept in check via our immune system, which chemotherapy utterly destroys, as the purpose of chemotherapy is to kill all dividing cells in the body, which is what cancer is. But at the same time, it also kills of the immune system, so when that happens, all the nasties then have an opportunity to come out and play. And so, once the chemo is finished, out come all the nasties to play. Thankfully, the one that I had thought might still rear its ugly head, never did. Hepatitis.
All through my time at the hospital I have remained reasonably active and mobile. I was quite often out and about the hospital, down in the foyer and other places, just to relieve the boredom. After the incident with the E. coli, Sally put a travel ban on me. She explained that my immune system was shot to pieces and so I was open to any virus that was going around, and we still had a pretty nasty flu season going on. So as long as I stayed on ward that was fine but going past the day therapy was out of bounds. It was a little more relaxed in the weekend as the day therapy area was empty. Also, another person I ran into whilst I was in hospital was our neighbour from across the road. He was not even aware that I had been ill. So I told him the whole story and he was shocked, but said since he was a painter at the hospital he would call in and see how I was doing, so he made me feel a lot better. So life in 2E dragged on. Nights were the worst, as it was when I was the loneliest and no matter what, after 8pm it felt really lonely as you hardly saw anyone past that point.
Another part of dividing cell culture in the body is hair. Ergo, when you see patients that have either chemo or radiation therapy, they have no hair and like most things with this sort of treatment, the changes are very subtle to begin with… just a bit of hair on the pillow every now and again, and the fact your hair is drying out and no amount shampoo works anymore is usually an indicator that your hair is gone. On about week 3, I realised the time had come to go bald, and got Karen to bring in the clippers and shave my hair off. The beard had gone a few days before that. Of all the things I missed during this period, it was hair I missed the most.
At this time we got a new specialist on ward, Peter Wood. He was amazing and came with a pretty loose approach to things, but he was rated pretty highly, and he made you feel comfortable due to his sense of humour. He seemed quite happy with the way I was progressing as my blood counts for platelets and neutrophils had got to their lowest point and that soon they would start to recover, once the chemo toxins left my body and then my bone marrow would kick back into business. In this time, I also learned about minimum levels for blood counts as to when they would do a plasma transfusion. If haemoglobin levels dropped below 80 (normal levels are 160) then you would get a blood transfusion, which takes 2 hours per bag to transfuse, or if platelets dropped below 10 (normal is 390), then they would give a bag of platelets, which takes around 30 minutes to transfuse.
So every day my blood was tested to see where I was and then they would tell you the results as to where you are and then what the plan for the day was. The only thing that cannot be transfused was neutrophils (white cells) and they really hit rock bottom. When they go down, they drop to zero, when between 2.5 to 5 is normal. The white cell count was the most critical out of the three, as they are the ones that fight infection, and without them I would pick up anything that was going around, hence why I had the separate room. Once they dropped below 1, I was deemed to be neutropenic and as such a high-risk patient. In fact, I had a ban put on me from leaving the ward during the week as I could run into people who had the flu and then I would really be sick.
The platelets were not so much of an issue as they are the clotting agents in the blood and can be transfused into the bloodstream, and it seemed every 2 to 3 days I had a transfusion of some description, or I had both on the same day. Two weeks after coming off chemo I was informed that there should be a change in my blood counts and they should be starting to turn around in the next few days and start heading back up, and once my neutrophils hit .50, then I could be discharged. I started on an injection every night, called GCSF, which is a bone marrow stimulant, which was supposed to boost my bone marrow into producing properly. It was usually administered by the trainee nurses as it was considered good practice for them in no matter what ward they ended up in. So I would mark them as to how much they would hurt when I was injected, as it was really a painless injection. Only two failed the test.
Like the GCSF worked… not. I got to day 35 in hospital and Dr Woods came to the conclusion that my neutrophils and other blood counts were going to be very slow in recovering and a decision was made to discharge me with the neutrophils at .20, but I still had to come to the fast track clinic three times a week to see how everything was going. I was also given a bag of pills and 7 days’ supply of GCSF so I could inject myself at home, and off I went.
Home and recovery
I came home and started my three visits per week to the clinic, which I soon discovered was not a fast clinic. The only reason it was called fast track, was because our blood work was done urgently. Other than that, you would spend up to 2 to 3 hours there each day, but we had no choice but to be there. I met a lot of lovely people at the clinic and after a while a group us became known as ‘the usual suspects’, as we were there at the same time on the same days.
My blood counts continued to drag their feet in going anywhere and after 3 weeks it was decided to do a bone marrow biopsy to discover what was going on. Word had also come back about my transplant, which was being done at the Royal Brisbane & Women’s Hospital (the Royal), that they wanted another round of chemotherapy; a consolidation round, it’s called, started as soon as possible. It seems they were now calling the shots on my treatment.
The biopsy was performed and 2 days later I got some good news that I was officially in remission, that it was not leukaemia causing my blood count issues, but that my bone marrow was a lot worse off, prior to my induction chemo than had first been thought, and that’s why my counts were so slow at coming up. At this time Karen’s sister, Barbara, came over for a week’s holiday, which had been pre-planned earlier in the year prior to this all starting, and I felt sorry her, as everything had to revolve around my treatments, but we managed to have a reasonably good time anyway.
In mid September, I got an appointment to go to the Royal Brisbane to meet with a haematologist called Elango Pillai, who all the doctors at the PA had big raps on as top in his field, to discuss about my bone marrow transplant, and we were given all the facts and survival percentages, etc. He said that my case was not a case of having any other option but to have the transplant, and it needed to be done no later than the end November, as a matter of urgency, and that it had been determined that my brother was the best match for the transplant donor. So now everything was moving at a pace that was staggering. I was also told I would be in hospital for 3 to 5 weeks. So there we were, with all the info we needed.
Early in October it was decided to go ahead with my next round of chemo even though my platelets still wouldn’t come up to the required levels, and about a week later I started my next round of chemo, which was a lower dose of the same two chemo drugs that I had in my initial chemotherapy. It was called 5/2 consolidation and the cytarabine was infused through a pump that was attached to my picc line, and I was allowed to do this as an out-patient and I only had to go to out -atients for the two idarubicin infusions.
The only annoying part about the whole procedure was trying to sleep with the small bottle pump that was attached to me, but I managed to get through this almost. On Day 4, in the evening, I checked my temperatures, which had been the norm for me three times a day since my discharge, and my temp was sitting at 37.8 degrees. At 38, I was supposed to got straight to the Emergency Department. After as second check, 30 minutes, later produced the same result. I rang the ward at the hospital to get some advice and was told to go to the ED to get checked. We arrived and gained immediate admission to the ED and was promptly seen, due to the nature of my illness. After blood tests and some other tests, it was determined that the chemo drugs were causing my temperature spike and I was sent home.
The following morning, being a Saturday, I went to have my pump removed as my five days were up and so, once again, I was free from my chemo drugs and so hopefully life goes on. Yeah, right.
That night I checked my temperature and it hit 38 degrees and I thought great, and I thought I would check it out in 30 minutes, but still got the same result, so we rang for an ambulance and off to the PA we went, much to the chagrin of the paramedic who wanted to take me to Ipswich hospital, as it was closer. When we got the PA we went straight to triage, because, as a post-chemo patient, I was able to bypass the normal waiting spots and when I told the triage nurse my patient number, the paramedic finally understood why I came to the PA. The PA is one of the few Queensland hospitals to have electronic records, so can be accessed from anywhere in the hospital.
I was welcomed back, and Karen and I were put into ED and awaited assessment by an ED doctor. It took forever just to get blood tests and compared to how quickly I had been seen the night before I was stunned by how slow they were.
After five hours it was decided I was to be readmitted back into hospital as two low-grade fevers in 24 hours was one too many and off I went to ward 2E again and I arrived up there at 6am, tired , hungry, and pissed off. I finally got to see Kate, the young registrar who I had met during my early diagnosis again and she said that I was going to be put back on antibiotics to try and get my fever back down. I was back in the same four-bed room I was initially in on my first visit. I got a visit later on from another registrar who told me I would be in hospital until my blood counts started to pick back up again. I said that if that was the case, I would still be here when it was time to go for my bone marrow transplant as my counts rose very slowly. The arrogant young doctor said that it would probably be two weeks and I’d be out as that was the normal timeframe. I just laughed and went to sleep.

Karen came up in the afternoon to see how I was getting on and at that time I was still pretty pissed off, as the people in my ward were just annoying the hell out of me, and the fact I was back in hospital really just annoyed me as well. They then decided to move me back into a single room again, which made me happy, as I was going to be neutropenic in the next 24 hours, so I need to be isolated again and so it was back into the same room as I had been in previously. So there I was back in hospital, back on intravenous antibiotics, and pissed off.
The specialist haematologist was a guy called called Stephen Mallay, who everyone seemed to think was a great doctor, but I found him to be quite cold and very hard to talk to and very awkward. Getting any information out of him was like pulling teeth, but I was reunited with the great nursing staff and so it made me feel a little better. I also met with bone marrow liaison woman, Rosetta, who would act as a co-ordinator between the PA and the Royal Brisbane and she outlined what would happen next as far the transplant was concerned.
One bright spot out of all this was that two of the usual suspects, James and Brooke, were also back in hospital at the same time, so it was good to catch up with them and it also helped pass the time as well. The nurses became a bit frustrated with me though, because like before, I would go walkabout and on more than one occasion I was told off for being off ward and in a place I shouldn’t be.
It appears that I would be doing a three-day work up just prior to transplant, where I would be put through a range of tests for heart, breathing, skin, chest x-ray, meet the BMT co-ordinator, meet the nurses at the BMT/Haematology ward and, of course, have another bone marrow biopsy. Great, just what I needed… more tests, but then I suppose I am going to be put through the wringer on this procedure apparently.
So there I was sitting in the PA going through the paces of being bored and having blood tests, transfusions, when required, and trying hard to convince them I needed to be back at home not in hospital, but they weren’t having none of that, and even Karen was starting to feel the strain a bit from all that was going on.
At this time, to relieve the boredom, I got conned into playing a halloween trick on one of the nurses, as the person who had been first asked to do this, James, had been discharged. So, to add a bit of spice, I thought, ‘why not, it could be good for a laugh’. My main concern was that the person in question was pregnant and I thought if we scared the hell out of her she might go into labour, but then we were in a hospital, so how much harm could it do, but alas, it never came to pass as I too was discharged a couple of days later.
Finally, I convinced Dr Mallay to let me go home after two weeks as he came to the same conclusion as Dr Woods before him, that my blood counts were not going to rise to the required levels by the time I needed to do the transplant. So off home I went and waiting for me were the dates for my pre-transplant work up… two weeks before transplant, which has been set down for November 29. I also got a call from my brother, Micheal, to say he was coming up from NSW to do his pre-donor check-up, which was a similar work up to me. He asked me what I knew about the transplant process and I told him I had no idea, but I guess we were both going to find out.
I was back on three visits weekly to the fast track clinic, just to keep track of everything, where one of the usual suspects, Brooke, told me she was also having a transplant. She had ALL, another form of leukaemia, and her donor was from overseas, but she was not looking to have hers done until the new year.
I think there were quite a few people in the waiting room that day who silently hoped all went well for the two of us, as it is a sort of a last resort option for cancer patients, when all other avenues of treatment have been exhausted.
On the prescribed day, Karen and I turned up at the Royal Brisbane Hospital for my pre-flight check-up that started at the dentist. I did breathing tests and finally met Judi Cummings, the BMT co-ordinator. Her job was to explain to us what was going to happen before, during, and after transplant, which she did, and then to sum it all up we were informed that I required a constant carer after my discharge from hospital up to Day 100 post-BMT.
We again sat there in stunned silence, because here we on the eve of the transplant having this bombshell dropped on us and then being told no carer, no transplant. I quietly informed her that Karen would be my carer and that was the end of that. She said did we not have family or friends that could help out too? No, they all work or live in New Zealand. I stopped listening to the silly woman after that and went through all the process of how we make this happen.
Following that, we met the social worker, nurses up at ward 5C, where I would be housed during my stay, and went home. The next day I had to do blood work, 12 vials of blood, and I was given a large container to pee in for 12 hours, and a small stool collection jar, and asked to return them the next day when I came for the biopsy.
Transplant time
So, all was set for my transplant. On the 22nd I went back to hospital to get my Hickman line inserted. It’s a rather horrible central line that sits just under the skin and goes into the jugular on the right-hand side of the chest. I also started the last round of chemo, another chemo drug, called fludarabine, for which I would have to go to hospital every day up until the 27th ,when I would be finally admitted to hospital for the next three weeks.
Off we went every day for my chemo, which only took about 45 mins to be infused, but you could spend up to two hours waiting for a chair or a bed. I had become quite adept at sitting in waiting rooms, waiting, but I was always fascinated with the impatience of a lot of people who thought that because they were told to be at the hospital at a certain time then that was when their appointment was. At the same time, my brother, the donor, had also come back to Brisbane in preparation to donate his stem cells for my transplant.
Apparently, he had to have a needle inserted into each of his arms where over the next five hours they would draw blood from him, centrifuge the blood to separate the bone marrow from the blood and prepare it for my transplant. We actually met up one day at the hospital whilst I was having my chemo and then I also had to have a blood transfusion, so we spent a good 2 to 3 hours going through everything that had happened since they had been up here in May. It was strange how everything had turned out to be how it was in such a short span of time.
Into hospital I went once more, into ward 5C at the Royal Brisbane and Women’s Hospital for hopefully my last hospital stay. This time it was for 3 to 5 weeks, depending on how well I responded to all the treatments that were going to be rained down my poor abused body. I had my last bit of chemo with the fludarabine prior to my admission and then it was of up into the bowels of the RBWH.
I still had one more dose of chemo to be done before my transplant on the 29th of November, a particularly nasty chemo drug called, melphalan, which is designed to kill of any remaining remnants of my bone marrow… like after all that’d been done to me prior had not finished it off. So on the 29th it was to be done, which would give me a day to recover before my transplant.
It’s a particularly hard regimen this last lot, where prior to having what was basically two rather large injections, I was dosed up with approximately three litres of fluids, then given a drug so I could then urinate it all out again. Apparently, it’s to ensure your kidney function is ok and no damage is going to be done to your kidneys during the procedure. Then they inject the two syringes of melphalan in through my Hickman line over a 10 to 15 minute period. All the while, I have to suck on ice cubes for an hour. This to prevent mouth ulcers that you can get from the infusion, such is the toxicity of the drug. I still can’t stand ice cubes to this day, as by the time the hour is up, you are gagging on them.
Then once I had finished the hour, I was again dosed up with another three litres of fluids, given the same drugs as before to help me urinate all the fluids out and to flush the melphalan out of my body as well. By then I was absolutely buggered and fell asleep for the next 12 hours.
When I woke the next day, I just felt wasted… like every part of my body was drained and I went through the motions on that day and was happy to not have anything else done to me. I met my new haematologist registrars that day. A young man, called Nick, and a young woman, Erin, who stayed on ward for the entire time I was a patient and I met the senior haematologist, Glen Kennedy.
Again, being on ward, I met some wonderful people who were also going through or had been through the same procedure as myself, and so it was good to talk to people who were in the same boat as me. In particular, I met Terry and his wife, Jo. He was a day behind me in transplant, but his donor was from overseas. He was a very nice man of a similar age to me and Jo was a lovely person as well and, like me, this had been thrust on them at such a pace that it made your head spin. Another was my neighbour in the next room, Merrilyn, who was on her second transplant in two years. Another I met, after Merrilyn, was a lovely lady, Dianne, who was in for her second round of chemo in 18 months. It appears she had relapsed and so had no other option but to have a bone marrow transplant, which, as an older person, had a very low success rate, but before that she went through absolute hell with the chemo she went through. I was so lucky up to this point that I had not had any issues. I also started a lot of the drugs I would need to take post-transplant, to help it work … hopefully. There is still a chance that the transplant may not take, and it could take up 18 months for full engraftment to take place. One of those drugs was an immunosuppressant, called cyclosporin which was necessary to prevent GVHD (graft versus host disease).
The big day came, 29th November 2017, transplant day. Was I ready? As well I could be sure. Was I scared? You bet I was, but I knew I had no option but to go ahead. A lot of people had put in a lot of effort to get me to this point, my brother not the least amongst them. He came up to see how I was going, but the transplant was not set down to be done until the afternoon, so we chatted for a while and then Karen arrived as well. It was like everyone coming to see the condemned man one more time.
I was given phenergan, an antihistamine to stop any allergic reaction I may get from the transplant, and it was great stuff, like being stoned. I remember lying there, waiting for the nurses to come in for the transplant, and this silly woman who was the social worker came in to see me and I lay there thinking, ‘ lady I really don’t care what you are saying and I don’t have the cognitive facilities to concentrate either’. Around 3pm they came in to do the transplant, which was basically just like a blood transfusion. I asked the doctors prior to this how it worked, and they said the stem cells were placed into my bloodstream via the Hickman line, then the bone marrow cells would do the rest. It took about 11/2 hours to do the transplant and then I was left alone to sleep off the phenergan.
The next day was called Day 1 and all days following the transplant are numbered from there. On Day 1 I was given a low dose chemo drug call methotrexate, which is used to produce a reaction in my body between my body and the graft stem cells, and this would be done on Days 3, 6, and 11. During this time I still had no reaction to any treatment and so at one stage I was termed as the most boring patient on ward. Terry, who I had met at the start of my hospital stay, on the other hand, was going through absolute hell, and at one stage they were going to put him in ICU, because his symptoms and side effects were so bad that they thought he would need to be put in an induced coma just so they could feed him.
Meantime, I had a new neighbour, Dianne, who was in for her second round of chemo due to a relapse of her leukaemia and this time she was to have a transplant as well. Poor woman went through hell as well with her side effects being so extreme that she lost the best part of 13 kilos in a week.
On Day seven I was given a GCSF injection the same as I had had following my initial chemo treatment, and this time it time it certainly worked and I was introduced to a new pain, bone pain, caused by the over production of my bone marrow. It also put my blood counts back to where they should be. I needed a strong pain killer and I was introduced to fentanyl. On the second they repeated the process and that was that. My blood counts were back to normal, so no more blood transfusions.
On Day 20 since my hospitalisation, I got what was called a ‘day pass’ and I was allowed to go home for the day. It is designed to see if you have any issues with getting infection or anything else in the home environment due to the fact that I have no immune system. If I got over this small hurdle, then I would be discharged the next day.
On Day 21 I finally got to go home with a bag full of medication and a very long rehab ahead of me with twice weekly visits to the hospital for blood tests and results and a plan of action going forward from there.
Discharge to Day 100 / 2018 – up to here
Thankfully, I was out for Christmas, which was a bonus, but due to the fact I was still not very well it was a very subdued Christmas Day. As I said, I had to go to hospital twice a week to do blood tests and adjust my cyclosporin levels according to those test results. The level of dosage was dropped reasonably quickly over the first month to a level that was maintained over the next few months. All my tests came back ok, and I continued to make solid progress and I remained bored as I was not really active due to certain restraints placed upon me by my rehab.
The days just seemed to go along, and the only break in my boring routine was the hospital visits and we did manage to go into Brisbane on the odd occasion but I still remained a little fatigued by what had happened to me in the previous four months. At least I was still alive, that was the main thing.
Day 100 was in the middle of March 2018, so I had to redo all the tests I had done prior to my transplant, so it was off to the dentist, skin clinic, breathing and bone marrow biopsy and I would also have my Hickman line removed, hopefully. During this time, I also ran into Brooke again, who as I mentioned earlier I had met at the PA when I did my original chemotherapy. She was about to go through all the tests and everything prior to her having her bone marrow transplant. She looked quite scared as I can remember how I was, so I sort of became a sort of support crew for her on her journey.
At Day 100 I finally got the results of all my tests and I remained in remission which was the result we were all looking for. I also, after much pulling and cutting of skin, had my Hickman line removed and I was finally free of my lines and now all my blood work was to be done by needles. I was also put on to fortnightly visits to the hospital which also made me happy too, but I now had a lot of free time. Karen returned to work after my Day 100 results and I was left alone. The other great thing that happened was my hair started to grow back, and when it came, it came back with a vengeance. I have never seen leg or arm hair so long, and my head came back all nice and black and soft. I really did not enjoy not having any hair, and I called myself Kojak on more than one occasion.
Day 101 to return to work
From this point, I was deemed to be not in any danger and so Karen returned to work and I went about the business of filling in my days with some cycling, a little golf down at the driving range, and my fortnightly visits to the hospital for blood test results.
In mid May, I thought I would take a punt on using public transport to get to the hospital and back to save on the exorbitant parking fees that we were being charged just to be sick.
After an initial trial, and wearing a mask, I decided that it was far cheaper to take the train in and so I got to save a lot of money on transport costs, and also I had dropped a few of the medications I was taking as well.
During this time a friend of mine, Rob, who is on a disability pension rang and we got in contact over the weeks and met up a few times for coffee, and to go to the driving range. He had to have a couple of operations in 2018 and so I was able to support him and go visit him during this period.
Other than that, it was a pretty boring and lonely time for me, and every now and again I would go into work to catch up on work colleagues and just to let them know where I was up to with my treatment. In the middle of June, I had another bone marrow biopsy for my six-month post-transplant check-up. Again, it came back all clear and I was also informed that I could return to work when I was ready. I explained to Elango that I was not too keen to go back in the middle of winter, especially during flu season, and that I would prefer to wait to closer to the end of flu season. The joys of having no immune system is that all these things needed to be taken into consideration. I had already had four colds since March, and was not willing to go for number five off someone that had brought it to work.
I finally got to August, and during my visit to the hospital I was informed that I would now be on monthly visits and my cyclosporin which had falling steadily through the months was now down to 50 mg a day. So I decided it was time to return to work and see how I went.
I contacted work and we had a meeting the next day and agreed that I would return to work on a three-day-a-week basis for the first month and then see how I was tracking from there. I thought this was a good deal, and as I had been out of action for a year, I was not inclined at my age to want to do 40 hours straight up. Throughout this entire process the thing that has really been helpful was how understanding my employer was and that they were happy for me to be off for as long as I needed and they have continued to be since my return to work.
Return to work and beyond 2018
On August the 6th I walked back into work for the first time in 51 weeks and it felt really quite strange as I was not quite sure as to where or how I was going to fit back into the shift.
I started of doing three-day weeks for the first month as I still had hospital appointments and also fatigue issues, from the chemo and transplant, and for a while I really struggled to get to the pace of being back in the whole environment. The heat was my biggest problem, as the industry I work in is a very hot industry, at the best of times, and then add in the spring/summer heat and it became a real toil, both in the lead up to Christmas and following into the new year and the hottest part of the Queensland summer.
I also felt at this time that I might be struggling with a bit of depression as I was struggling to fit in at work and so in the end I went to see a psychologist about my problem. What he told me was that due to the nature of what I had been through, I was a totally different person and that was what I having problems with, the new me struggling with my old self, and that in time I would work it out. But it was going to take time and for me not to worry too much about it.
At the end of November, I had my 12-month work up post-BMT and on the 29th of November I celebrated my one year re-birthday, as some people like to call it for those that have a BMT. All my results came back clear, which was a huge relief, because those tests and the bone marrow biopsy are particularly stressful, especially if you have not been feeling too flash in the period before that. I also lost the bad tooth that I had issues with right through my induction chemo and transplant and that was also a great relief, as it had really started to affect my health as well.
I was also informed that I was dropping the cyclosporin after being on that for 12 months, and also a range of other medications I had been on, which made me happy, as I felt that by coming of these pills I was heading in the right direction… not to be.
2019
In January, I started to feel some discomfit in the joints in my hands and a light rash starting to appear on my arms. I mentioned this to my haematologist and he said it looked like I might be having minor GVHD issues, so he recommended I go back on a low dose of cyclosporine, 25mg per week, and we’d see how that would go. I also got my first round off vaccinations done. So with that, coupled with the immunosuppressants, I actually started to feel I was heading in the right direction.
As I was going along fine I was also put in touch with a closed group on Facebook for AML sufferers which once I joined has turned out to be a great source of information, as nobody knows and understands the nature of an illness better that others that are going through the same illness and so I have learned a lot from this group and have passed on my own experiences as well. This has been as much of a valuable tool to me as it is talking to the so called experts who deal with the disease and not the other bits that come up along the way.
In April I suffered a bit a setback when I came down with shingles, which was not a lot of fun as I had the rash and blisters in my mouth, on my tongue, down my throat, on the outside of my face, and up around my ear. All this was on the right side of my face, so I was eating soup and mushy food as it was too painful to eat to solid food. I was also put on a high dosage of valacyclovir, an anti-viral I had been taking during and following the transplant. It was seven days of six pills per day and since then I have been on them on an ongoing basis.
It also cost me nine days off work, which was not ideal as we were struggling financially, as some the debts we had to rack up whilst I was off work was now starting to catch up with us. So only working a grand total of six days in April, due to the illness and public holidays, certainly took its toll on not only me but Karen as well.
Unfortunately, it left me with this great new thing that I had never experienced before – nerve pain – which made it difficult to sleep on my right side and very difficult to shave as well. I started to look like a homeless person as the top of my head was sensitive and a haircut was not going to happen anytime soon. As the blisters were starting to abate, I went to see Elango and he put me on prednisone to reduce the swelling in my ear. Due to the shingles, I could not have my next round of vaccinations, so they were delayed another month and we would look at it then. It was also noted that there was an increase in iron in my blood work and that my liver enzyme tests were coming back a little high. Elango thought it might be due to the valacyclovir and the fact I had been subjected to number of viruses and the use of antibiotics to counter their effects may have contributed to it as well, or it could be GVHD, so he increased my cyclosporine to one every other day and we would see what was happening when I came back in May.
So off I went home, feeling a little down but still optimistic I was heading in the right direction.
Early in May I came down with a cold and so by the time I got to my next appointment I had been on antibiotics for about four days, so my vaccinations were once again delayed. At the same time, my liver enzyme tests had actually gotten worse and so had my iron, which had increased, so there was some concern shown by Elango, as he was at a loss as to what could be the problem. I also asked what my status was regarding my hepatitis B. I had been a carrier all my life and had been on hep B suppressant drugs right through my chemo and my BMT. He sent me off with a blood form to get my hepatitis status checked.
In late May/early June I suffered from another viral infection, this time in my sinuses and at the same time I was also having GVHD issues with my lungs, so I generally felt like shit, but I soldiered on at work and everywhere else. I went back to the see Elango in early June and he said preliminary results showed that my hep B was ok but he was waiting for the final results and if there was a problem he would call me straight away. Well, there was a problem, because he rang back within a week to let me know that the hep B had become active for the first time in my life and that I needed to go back on to hep B suppressant medication. He then rang back later in the week and asked me to get some more blood tests, but could I get them done at the pathology dept at the hospital. While all that is going on, I’m still coughing and feeling like crap, and at work we are facing an uncertain future as we need to lay off at least 70 people. So that is adding even more stress to a situation that is really just starting to drag me down a bit.
I managed to survive the cull at work, but it still was a tense time, so I embarked on a period of time where I pushed my body a bit and boy did it push back. As I was still recovering from the hepatitis and all the other things that had gone wrong during the previous months, I tried to explain to people at work that I was far from being right and that I would never be the same worker I had been prior to my diagnosis. But it seemed to fall on deaf ears and they assumed, and one even said to me, that I was using my cancer diagnosis as an excuse to not return to the normal duties I had done prior. To say I was stunned by that statement would be an understatement. We were all assigned extra duties to perform, as we were now a reduced work force and so these extra duties although not much, increased the fatigue issues I already had, with most nights me falling asleep in my chair whilst watching TV.
I guess that all the punishment my body had been put through during the chemo, transplant and my recovery was going to have a permanent effect on me. I just wish that the doctors and advisers I had at the start had warned me that this was going to happen, but their only concern is my treatment and eventual recovery and the physical and mental things is a side effect. Not that it would have changed my mind in the least about going down that path.
During all of this my cousin, Paul, who had been a real tower of strength to me, had also been battling his own cancer. His was much worse than mine, as he had a Stage 4 glioblastoma multiform, or a terminal brain tumour, and it pales in comparison to what I have gone through.
I also discovered, as I have come off medication that there is a now a tingling in my fingers and toes, and sometimes they are just numb, and I have a numb patch on the left side of my face, between the eye and my mouth, and on my cheek. When I had the first incident that started all of this, it was this numbness on the side of my face which led them to believe that I’d had a TIA , but it turns out it is peripheral neuropathy, which is a dulling of the nerves in the nerve endings. It can also lead to bad cramps in the hands and feet, which is really quite weird, and takes some getting to used to.
It appears that this is a result not only from the AML, but also a result of all the damage that is done to the body following chemotherapy and that this will be the norm for me for the rest of my life as there no treatment for it. So life must go on. One of the more delightful side effects from this is also dizziness, which is to say the least, is the most disturbing one of all.
Especially with my job of being a machine operator that stands in front of a machine that had the ability to do some serious damage to your body if you get it wrong. But it also produces metal at a temperature of around 530 degrees plus, so it can really hurt you. So, to have someone with erratic dizzy spells standing in front of this sort of carry on is not a good idea. I passed this very serious info on to my manager so that they were aware that in the new year I couldn’t carry on doing that job that I have done for over 40 years. He was more than sympathetic and said maybe it was time to re skill myself in different elements of my industry and so that is the plan for 2020. Leave it to younger people to do the hard yards, as I feel I have nothing left to prove and I can slowly slip into a sort of semi-retirement, so to speak. I’m sure this will go down like a lead balloon to some people, but then I’ve got to the point where I really don’t care what lot of people think anymore.
By mid September to early October ,my blood work showed that my liver function was slowly returning to normal and that my iron, that had been at an abnormally high levels for well over two years was all coming back into normal ranges and so I looked to the future where my health issues of the last two years were slowly fading into the past and I could look the forward with some positivity. I was even adapting to the tough regimen I had with the hepatitis suppressant pill that I’m required to take for the rest of my life… or so thought.
On November the 28th I had my annual bone marrow biopsy as required. It had been two years since transplant, so it needed to be checked to see if there are any anomalies, etc and to check the health of the transplant.
On the following Monday evening I got a call at work from Elango to tell me that they had found some mild form of dysplasia in my marrow, but not to be unduly alarmed as he would wait for the final test results at the end of the week and then take it from there, but in the interim for me to come off cyclosporine. I informed him I had been off cyclosporine for the last month as he had given me an option to reduce to one tablet a week or stop it completely and I took option B.
Relapse to MDS and beyond
I was not unduly concerned at this stage because I did not know the percentage of blast cells in my marrow, so I went about my daily tasks and pushed it out of my mind until I got the final results. On Thursday I finally got the news all cancer patients fear to hear. I had relapsed, not back to AML, but to MDS, the original diagnosis I had before it morphed into AML. I sat out the back of the factory like a stunned mullet, not believing what I had just been told, but trying also to process what this meant. I went and told Karen the shocking news and then we went and met with my manager to also let him know that things had taken a turn for the worse. Again.
Although MDS is not as bad as AML, it is a precursor to it and requires, in most cases, some form of treatment. Some people go on a watch and see approach as it can sit in your body for years and do absolutely nothing. Others like me…. unknown.
I informed my manager that I had to have blood tests the next day and because my head space was not exactly good that I would take the next day of as well. So off to hospital we went the next day all bright and early as I got the impression on the Thursday that the blood tests were rather important, and seven vials of blood later it was all over. We spent the rest of the day processing the news and I had an important call to my brother, as I was told we may need some T-cells from him some time in the future.
The blood tests were to check whether I had chimerism, whatever the hell that is. I did a quick Google search and it revealed that chimerism is the art of having two DNA profiles at the same time.
Apparently it can be a rare but naturally occurring thing or it can be quite common among bone marrow transplant patients, as chemo did not completely destroy my own cells and about 5% of my marrow is still mine and the other 95% comes from my donor. Apparently, the results for these tests take some time to be finalised.
I already had an appointment on the following Wednesday to see Elango, so waiting for the appointment to come around was like nothing I have ever had before as we already knew sort of what was going on, but not what was going to happen as far as treatment was concerned.
On the day of the appointment I was told that my blast cells were at 13% and holding steady. Although it doesn’t sound like a high number, I was told it could sit at that level and go no higher, but they were not prepared to take that chance and there was a small window of opportunity to use a low strength chemo drug call azacitidine to treat this, because once the blast cells reached a certain level then a stronger more nasty form of chemo would then be the only solution left.
As I said earlier 5% of the marrow that I had was still my marrow, which had carried the MDS mutation in it, and apparently it was now coming back to haunt me and create all the havoc that now ensued.
I was to start this new treatment on Monday the 16th, which was only five days after my appointment with my doctor. I was told it entailed two injections in my stomach every day for seven days, then I had a 2½ week break, then the process was going to be repeated. Then, after three months a bone marrow biopsy would be conducted to see how effective the treatment had been. If I was back in remission then they would move on to the next phase of treatment, which Elango said was to make my bone marrow angry and try and induce some GVHD in me so that then it would activate some activity from my transplanted T-cells which had been very inactive which led to the MDS relapse in the first place.
There was also talk about using interferon, and I was unsure what that is and also T-cell replacement as well. Apparently all this is going to take an awful lot of time, so I was told it was better off if I did not try to go to work during this as it is a very time consuming treatment, although having 2½ weeks between treatments does sound like a lot of free time to do things.
I was devastated by the news and a whole pile of angry, but as Elango had explained, it could’ve been worse. I sat thinking, how could it be worse, until he explained that if I had not had the biopsy when I did then, it would have gone undetected in my system until it showed up in my blood work, by lowering blood counts, then I would have been back to square one, with AML and having to redo the induction chemo and bone marrow transplant. So yes, I guess I was lucky it was only MDS and it was only in the early stages and treatable easily too.
Elango was as devastated as I was about this turn of events and he said it was a result no-one saw coming as all year my blood work had been excellent and, although I had had the immunity issues through the year with shingles and the hepatitis thing, nothing was there to suggest this was going to happen.
I rang work to inform them that I would be off for the rest of the week and that I would be in the next day to fill them in on what was going on. On the Thursday morning I was feeling a whole heap down and I rang the HR manager to see if she was going to be in and whether I could see her. She immediately knew something was wrong and asked if I wanted her to come over. I just blurted out that I had relapsed, and I needed to talk. So my first port of call was to see her and there was so much sadness about the fact that this had happened again, but she was wonderful, told me to take as much time as I needed and just to get myself well again and when I was ready, come back to work.
She arranged all the forms for me to apply for income protection and all the company’s side of things, and for me to keep in touch through the whole thing. I next went to see Craig, and once again my conversation with him started with, unfortunately things are worse, and again told him I was off for another considerable length of time and he said the same as Mary-Anne (HR manager), take as long as I needed, and we would take it from there. They also agreed that Karen should have the last working week of the year off as it was unknown how the treatments would affect me.
On the Monday we headed off to hospital early as I needed to do blood tests again and I had another appointment with Elango before I started my treatment, so it was going to be a long day at the hospital, again. Once blood tests and the appointment were completed we sat and waited, for over 90 minutes to finally go in and start my treatment, which is basically two jabs in my stomach, but they have to be in different places each day and they leave a rash and last, but not least, they hurt a little too if they are not done properly.
And so that was my routine for the next seven days, right up to Christmas Eve – hospital every day, two jabs in the stomach, and home again. At least this round of chemo was not as harsh as the last one, so there was a limited amount of nausea and I have not been left feeling to out of kilter, and so life just goes on. My next round of treatment begins on the 13th of January, so I have to do it all over again.
Income protection battle
During this time, I applied for my income protection insurance to kick in so that at least I would have some form of income during my treatment period. I put the application in on the 17th of December knowing that it was a difficult time of the year and that any decision on my claim would not be forth coming before the Christmas/ New Year period was over but I thought by mid January that I would have an answer. On the 24th of December I received an e mail asking me to get 3 years of my medicare records and instructions on how to go about. The email also said it would probably take 2 days to gather all there data as things had to be set up in My Gov before I could proceed….. 15 mins later I had everything I needed as I already had My Gov account and so I promptly e mailed all the data back to them…. Teach them to pull that crap on me on Christmas eve.
2020
On January the 3rd I received another email form the assessors from the insurance people claiming extra medical data needed to be gathered and that forms had been sent both to my GP and to my specialist and if I could get those forms filled out and returned ASAP then that would help move my claim along a bit quicker. So off to the doctors I went, to see my GP on the 5th of Jan to help her fill out forms which on most questions, she had no idea of the answer as those questions could only be answered by my specialist. I felt sorry for her and she did the best she could.
I rang the hospital on the Monday to see if I could get Elango to fill out the forms as quickly as he possibly could but I understood that he is a busy man and has more than me to worry about, so it did not surprise me when rang me on the Tuesday mid-morning to inform me that he had not received any forms from the insurance people.
This came as no surprise to me, so I rang my assessor to inform him that Elango has not received the files and he asked me for his email address or his phone number. I said I did not have these as when Elango needs to contact me he rang from a NO CALLER ID number, and if I needed to contact him I left a message at the haematology desk for him to call me when he could.
For two weeks I heard nothing and on the 14th of January I rang my assessor to find out what was going on, only to be informed the forms I had filled out on the 5th were only just being returned to them by my GP. I rang the office of my GP to find out why there was a delay in sending the forms back to the assessor. Apparently, it came down to a matter of payment. In other words, if they wanted the reports then they had to pay my doctor for them. Also, they said there was a delay in getting the documents from the hospital, a delay they created. I think that they think everyone is at their beck and call, not realising that my specialist is also an extremely busy person as well. And that was the last communication I had from them for some weeks.
During all this I had been keeping Mary-Anne updated via all the emails I sent to them and by her calling me and so she also took up the baton and started chasing up Chifleys, with whom I have the policy and one that is not only supported by Capral but by the AWU as well. So she was in contact with people at the company and they were also becoming frustrated by how long this thing was taking and they were pushing to have it sent to another assessor to try and get this pushed along a bit faster. Still no decision was forthcoming, and on the 27th of January I got the call from Mary-Anne to prepare myself to the fact they may be going to decline my claim. She, like myself, and her contact at Chifleys were still trying to figure out what was going on as this was a new diagnosis not a relapse as the condition I had, although a leukaemia, it is not the same as the nasty one I had before.
At this time it was suggested to me that I get in contact with A Current Affair and see what they could do for me as it seems if the insurance company wanted to play hard ball then maybe it was time for me to also do the same. I dropped them a line and explained what was going on, but have never heard back from them, but it was also filtered back to the insurance company that I had been in contact with them and that put the wind up them a bit, and they were confused as to why I would do that. Desperate times call for desperate measures. I also let it be known that I had also been in contact with AFCA, the Australian Financial Complaints Authority, as well. All of this was designed to show that they were not the only one who could apply pressure and I think they were hoping I was just going to drop the claim. Fat chance of that happening.
So here I am battling a disease that I thought I was done with, but also battling an insurance company with whom I pay premiums too and they just seem to be dragging their heels in approving what should be a simple claim. I’m sick and can’t work due to treatment. Pay me what I’m owed… simple. I have never been so low in my mental strength and this has really tested me and there have certainly been some dark times in this process. Still, I march on slowly hoping that they will make a decision soon as it has been over 60 days since I stopped work and I finally I got an email on the 3rd of February to say that all the medical files had finally arrived the previous week and that I would get another update on the 14th, whether there was decision or not. So that just adds more stress to the issue as I have no leave left. We have some savings and I don’t want to have use it all, and I may be forced to return to work just so we have some income whilst these people muck us around.
The thing that threw a spanner in the works was that on the previous week Elango sent them a letter that stated that I was in remission and that two prior bone marrow biopsies in 2018 had shown that I was disease-free and that although MDS is a form of leukaemia it was not the same as AML and because MDS has no set treatment, as it is a moving target, he cannot state with any certainty how long I will be off work for or if I will ever return to work.
Finally on the 6th of February I got a call from Mary-Anne saying they were still trying to make a decision on my claim and it was now coming down to manifestation of the illness and it was just another road block the was being thrown up after everything else had failed. She got another call and said she would ring me back as soon as she was finished, which was about two minutes later. The other call had been from her sources inside – the insurance people – and they had rung her to inform the claim was finally accepted.
At last, I could now move froward with my treatments and not have to worry about the insurance thing and even though the income I would receive would not be a good as my normal wage it is certainly going to be better than 85% of nothing, which is still nothing.
And so on the 17th of Feb I started round three of azacitidine and wasn’t that Monday an absolute shocker. I turned up at 8.30am for my appointment/review with Elango and got to see him at about 9.20am but luckily my treatment wasn’t due until 10’ish. By 12.30pm I was starting to get a little pissed off as I had to pick Karen up from work at 2pm and by 1.45 I knew she was just going to have to figure it out as that is when I finally got called in to do my two injections… 5¼ hour wait for two injections that take basically 10 minutes to administer. I sent her a text to tell her I would be late as I still had to catch the train home and then get to work to pick her up. In all this time, I had hardly eaten and so I rushed to pick her up and so we finally got home at 4pm and decided to have takeaway for tea as we were both pretty buggered and couldn’t be bothered cooking. We had tea and an hour later I threw up most of mine as my stomach was so empty the food I had was far too heavy.
Anyway, the rest of the week went remarkably well. I was in and out of the hospital within an hour, except for Friday, which was just over an hour and it looked like an omen for things to come after that. I stopped at a cafe across from the hospital for a coffee and a bite to eat and after 25 minutes I had to ask where my food was. They had forgotten, but I got a free coffee out of it.
So I finally got home at 12.30pm and I thought at least it was not as bad as Monday and I would be able to pick up Karen from work on time. Yeah right. I left to go and pick up Karen from work at 1.30pm and as I came out on to the Cunningham Highway I was confronted by a long line of traffic going nowhere. Apparently, there had been a truck rollover further up the road, and so there I was again calling here at 1.55pm to inform here I was going to be late. Fortunately for me the off-ramp I had used was only 100 metres up the road and after about 30 minutes the police started diverting traffic back up there, so it was a swift three-point turn back up to the off-ramp and finally I got to pick up Karen just after 3pm. What an absolutely shocking week.
I was told by one of the nurses, who was also not happy about the fact that I had spent hours waiting on the Monday, to provide the hospital with some feedback as they tended not to believe the nursing staff when they passed this sort of thing on to them.
So I got on the Royal’s website and provided feedback. I wasn’t nasty, but I pointed out that there had to better ways of dealing with patients like me whose treatment took less than 30 minutes to complete, and about two weeks later I got a call from Elango. Apparently, as my specialist it was up to him to provide me with the answers to my feedback, and as I explained it was not a complaint but a concern, and he was also annoyed that this situation had unfolded for me as it did and they were going to review how people like me are handled in the future because, as he said, it’s all about listening to patients and their concerns as well. He also told me that he was happy with the way the treatment was heading and the that fact that my blood counts are holding steady during treatment showed that the treatment was working but he would wait for a biopsy to confirm that this was the case and that I still had three more rounds of azacitidine to complete before we started the next phase of my treatment for MDS. Bugger, more bloody needles.
COVID-19 and treatment, biopsy
In late December 2019, a new virus popped up on the radar, originating from Wuhan in China. It was a coronavirus which meant it basically attacks anybody with a piss poor immune system or anyone over a certain age. At first it was contained inside China, but most countries and yours truly did not take a lot of notice about it until people started dying and it then moved about the globe at a good rate, and although at this point of time near the end of March, there only about 500,000 cases out of a population of approximately six billion people, and a mortality rate of approximately 3.6% , the whole world has gone absolutely nuts trying to prevent the spread of this virus.
They have shut countries down, stopped people from travelling and social interaction and even introduced social distancing of 1.5 metres between people. Through all this madness, I still have to keep up with my azacitidine injections and on March the 2nd I had my eight bone marrow biopsy. I must be up for a set of steak knives by now or some special prize for enduring that sort of thing.
A week later, on March 9, I got the results which showed my MDS is in retreat which means the azacitidine is working in controlling the disease. I ran into an old friend, in the form of the registrar. It was Kate Hill who had been one of the doctors that I saw at the PA when all this drama began and she was there when I received my original diagnosis for AML in August 2017. So she was grilling me a bit about how things had unfolded and she could see that the blood counts and everything last year were good and she agreed that it was unfortunate that I found myself in this predicament.
But here I was, in this predicament and so off to treatment I went for another seven days. If I said I was not going to have any drama this time, I would have been telling lies because once again I found myself on the wrong side of another error. This time at check-in, where I presented myself to check in, the nurse never did it properly, so after 90 minutes I told the nurse I was going for coffee and when I returned I thought I would check to see how long I would be waiting as it had already been 90 minutes, only to be told that I had not yet checked in. Then the shit hit the fan again and within 10 mins I was in, injected, and on the way out the door and off home.
I have had a terrible time with this 4th round of aza, as the right side of stomach has become very sensitive and every time I was injected it hurt and hence the worst was yet to come. Normally, after seven days injections, my stomach is bruised and very red, but normally by the weekend it has all settled down and I’m starting to recover, so my body is ready for the next lot of abuse it is going to get. This time the last four injection sites have been quite inflamed and extremely sore for the next 12 days and my stomach will only be returning to some semblance of normality by the time the fifth round is started. I was that concerned about this that on the 26th of March I went to the hospital to get the sites checked out, just in case there was some other underlying reason why they were not healing. The doctor was really concerned by it and gave me a script to get some steroid-based cream for the swelling and inflammation.
By the time the fifth round began on 6/4/2020, the sore wounds from my last cycle, which had finished 2½ weeks prior, had just settled, and so off I went once again. Some of the shots I had did not settle very well, especially those below the belly button, and after five rounds I figured out what part of the problem was. The lower injections were either rubbing on the belt from my jeans or from the seatbelts in the car. They were in the exact position that the seat belt was when it is connected. Armed with this knowledge, I will ensure that the injections are higher and if need be, injected into my thigh instead, to reduce the issues I am having.
Luckily, I have a slightly longer break between cycles and so the extra week I get will also help my poor abused stomach heal, but there still remains some lumps, which I am also hoping will be gone as well.
The toughest thing I have had to deal with has been isolation as with the COVID-19 bullshit going on, all the places I was able to visit last time, like the art gallery, the museum, and other places are all closed, and with the issues with my stomach after round four, I couldn’t ride my bike or play golf as I was in so much discomfit I was taking 10 panadols a day just to keep the pain at a reasonable level.
It was only 10 days after I had finished cycle five that I was able to go to golf and have since started riding my bike, as along with the isolation/depression issues I had, cycle five also took a physical toll as well, and issues like chronic fatigue have also kicked in. In some ways, this form of chemo is actually harder on the body, than the induction/consolidation chemo was for my initial AML.
I even mentioned that to the nurses who administer my injections, that this is a more taxing regimen than induction chemo and they were surprised to hear that. They were led to believe that it was not that bad, but one nurse, Ingrid, tended to follow along with my thinking, and said there had to be a better way of doing this, than how it is currently being done.
The fatigue issues are the worst, as it just leaves you feeling drained and I went to a exercise physiologist to get some exercises to try and combat the issue a bit, but it can only slightly control the problem, not fix it, as the fatigue is a result of all the treatment my body has been through and will be my constant companion for the rest of my life. I am just going to have to manage it as best I can and listen to what my body is telling me, which to this point I have not really done effectively, but I will continue to work on it.
I remember having an interesting discussion with one of my work mates about being fatigued. When I was asked why I didn’t do as much as I used to and why I felt I needed to be treated differently to all the others, I told him I suffered from chronic fatigue and his answer was that I should get more sleep. I explained to him that this was not a sleep issue but a deep muscle/bone fatigue and that no amount of sleep was ever going to fix this issue.
So on the 11th of May I will start, hopefully, my final round of azacitidine. I have an appointment with Elango, which will be my first with him since early February, and so then I might get some answers from him as to where my treatment is heading after I finish this next round and what I can expect next.
On the 7th of May, four days before I’m supposed to start my next round of azacitidine, I get a call from the hospital to tell me my haemoglobin count had dropped to 84, off my latest blood tests from the day before. It certainly was a reason as to why I had felt quite tired, listless, dizzy and lacking in stamina over the last couple of weeks. I was going to mention it on Monday when I saw Elango, but now I have all the facts, I’m better informed. The downside to it is that I now have to have a blood transfusion on Saturday, just to get my counts back into a reasonable condition.
Then I was also informed later in the day that Elango wants to do another bone marrow biopsy on Monday to try and nail down the exact cause of my blood counts dropping so low, as they have not been this low since the days before my transplant in November 2017. It is now a worry as to whether my AML has returned. Hope not, as that would mean having to go through all the chemo and transplant all over again, a prospect I’m not really looking forward to. Best not get too far ahead of myself. Let’s wait for the biopsy results first, then see what the plan of attack is going to be. The other question is, are they going to do my sixth cycle of azacitidine? All questions that will need to be answered in the coming days.
I had the biopsy on the 11th and also spoke with Elango concerning what could have gone wrong with the recovery of my blood counts. He said it was very rare for what has happened to me, to happen. He said it could one of two things, the first being that my dosage of azacitidine could be too high and it had suppressed my bone marrow from producing the right amount of blood cells, in which case we will drop the dosage on it and carry on as planned. The other cause is a bit more insidious, in that I may be heading back into AML and if that is the case then I will need to be hospitalised for five days to do some other form of chemo.
My blast cells would have to up around 20% for that to happen, so I hoping it is just too high a dosage of aza and not the other. I get the final results of my biopsy on the 12th. He said he would ring me a give me the results, as if I have to go into hospital then that will occur on the 13th, so they get this back under control ASAP.
Finally, I got the results from the biopsy 24 hours later than expected and to say it was an anxious 24 hours was an understatement. But as the old saying goes, no news is good news, and this time it proved to be quite true. The final results showed that my blast cells were down to 1%, which is a great result after only five cycles of azacitidine, compared to the six that I was supposed to have. It also meant that I did not have to have cycle six as the job was done. The reason why I required a blood transfusion was that the aza had done such a great job and has actually suppressed my bone marrow from working properly. But I’ll take that as a big win in my corner.
Moving forward, once my blood counts recover, I’ll move on to the next phase of my treatment and start on interferon, to provoke some GVHD in me and hopefully fire up my immune system. I will find out more once I get to see Elango and have a discussion on the road ahead.
Interferon and beyond
On May 20th, I finally got to talk to Elango about all that had transpired in the previous weeks, but he seemed happy that I was doing so well and explained what was going to happen next. He also explained that although I looked to be returning to normal, there was no clear evidence that my low blood counts was solely due to azacicidine, but then again he said it would be foolish to do one more cycle if after the last round, my blood counts had not recovered.
So he said he was going to push on with the next phase of my treatment plan which was to use a drug called interferon, which issued to provoke some GVHD. Again, it was an injection in the stomach. More bloody needles, but at least this is only once a week and is not as bad as the azacitidine. He also explained that I could develop a rash or have stomach issues as a result of this drug, but it was that exact effect that he is after. I could also develop flu-like symptoms which is a common side effect. I said, great, we are going through COVID-19 and he’s giving me a drug that mimics the exact same symptoms as that. Great.
Finally, after four weeks of injections of interferon I’ve got a minor form of GVHD, dry eyes. So hopefully this will be the beginning of a way forward for me, as I was starting to get worried that nothing was going to happen and then I was concerned as to what the future held for me. Apparently, I have two more injections to go before the next phase of my treatment. As someone recently said in a group I just joined, I am one big science experiment.
I have also been struggling with the symptoms that the interferon gives me, and some days I feel like absolute shit and also I have been struggling with a bit of depression as well, as I am essentially feeling ok and so I could be working, not sitting at home doing bugger all. I guess I just miss human companionship and so in the evenings when Karen is working, I get quite lonely.
I have kept myself amused a bit by playing golf every week and riding my bike at least three times a week, but as the winter months kick in and the nights close in, is when I feel at my lowest. But at least with my weekly hospital visits for a blood test and my injection, it does give me some variety.
As I said earlier, I recently joined a group of bone marrow transplant patients that has been set up by a lovely woman named Lyndell. It’s primarily for people who have had a transplant, is going to have one, or close family members. It was held as a Zoom meeting, first time I have ever used it. About 13 people showed up and we went about introducing ourselves and relating our tales about our disease and the road to transplant and post-transplant. It was really good to actually talk to and listen to people who had been through the same sort of thing, even though we all had different types of leukaemia and different forms of treatment.
We are hoping to get together about once a month for a chit chat about issues that revolve solely around transplant patients.
In the past few weeks, the tedium has become worse for me as all I do now is go to the hospital once a week for my injection and that is it. The rest of the time is spent doing some painting, exercising, and trying to find ways to kill the boredom that now pervades.
As the restrictions from COVID-19 are slowly being lifted and life starts to return to normal, whatever that may be, I still find that I struggle, mentally, with my situation, as there are not a lot of people out there that I can talk too. Karen continues to work. I’m still not allowed to return to work myself, and I’m beginning to wonder if I will ever return to work at any time. At 60, and being told you can never work again is not exactly the news I need to hear, and although I have not been told that, I know that in 2020, I will not be working a day at all in it.
Due to COVID restrictions I am not allowed to even go and visit people at work and so my mental health issues are slowly getting the better of me as I have far too much time on my hands, alone, to dwell on all the shit that as happened to me since December 2019.
Anyway the treatments continue to go well, and although there are still no signs of extreme GVHD, I continue to have issues with a loss of feeling in both my hands and my feet, which is quite a bizarre feeling, my dry eyes continue, and every now and again my stomach reminds me that it too is not happy with all that is being done to me. But besides all that, I continue to feel how I have always felt… quite healthy.
In the next few weeks, they are going to harvest some more cells from my donor, my brother, so that they can start to replenish my T-cells as they are where the problem lies. Apparently, the harvesting is the same process used when getting bone marrow for transplant. He’s not going to be too happy about that, but I did warn him at the beginning of June that this might be happening. It also looks like the interferon injections are going to be an indefinite thing, as they are keeping my disease under control which, as this thing goes along, I’ve come to understand this is the aim of the treatment, to control, as there is no cure for MDS, there is only control. And so the invasion of drugs, etc, into my body continues. I may complain a bit from time to time, but I look at it from this point of view… at least I’m still around to complain.
At times when I am low, which of late has been quite constantly, as certain realities kick in, I draw strength from my cousin Paul, who sadly passed away on Dec 31 2019 from Stage 4 brain cancer, in the strength and courage and positivity he displayed throughout his short but brutal disease, knowing full well that he only had a short time to live. He made the most of what time he had, and I think it is time for me to approach my treatment and my moving forward into whatever fate I have… good or bad.
DLI and beyond… maybe
As previously stated, my brother was finally able to get up to Queensland from New South Wales, once the border restrictions were lifted in early July. This COVID situation has played absolute havoc with a lot of things. But finally on August 2nd after a three-day trip from the south coast of NSW, he finally arrived in Brisbane so he could do work up on the 3rd of August at the RBWH. This was to ensure he was fit enough to have the collection of cells, which was set down for collection on the 10th.
At the same time, I had finally conceded defeat and admitted that I might need some professional help with the mental struggle I have been having with all that has gone on. Well, that was a waste of time, as the person I went to was one where her sage advice to me was I needed to find a way to drag myself out of the hole I found myself in. Although she claimed to work with cancer patients all the time, I found she was a bit of a strange person. Thankfully, I didn’t have to pay for that piece of advice.
On the 10th, I turned up at the hospital with the express intent of getting my DLI sometime in the afternoon. The plan had been to collect the plasma from my brother in the morning and do a fresh transfusion in the afternoon. The problem was that my brother was a bit stressed out and so it took all day to collect the cells. So early in the afternoon we went home, and it was decided I would come back the next day and do the DLI. On the Tuesday I finally got my DLI, and then all the fun began. All went well for a few days, I was just a little fatigued but not much else. On the Thursday I went and played golf, and in their infinite wisdom they were burning some tree trunks and it set off my asthma. When I decided to bring this to the attention of the club, the owner decided that the problem I had was of my own creation, as since I had issues like the asthma and the cancer problems then I should have checked out the course condition before I teed off. Suffice to say that with an attitude like this, I am no longer a member of this course.
On the Sunday, I started to feel an increased tightness in my chest and some difficulty in breathing, but it was not asthma-related. By the Monday it got increasingly worse, so I attributed it some form of GVHD and I rang the hospital to get some advice. They told me to come straight in as my symptoms were a bit disturbing. I rang Karen at work to come home and take me straight to hospital and so off we went and after three hours of tests they could not find anything wrong with me.
The following week I started on my 6th round of azacitidine, which I was not looking forward to starting again. I was told it was only going to be a half dose, or only a single injection per day, but this was changed at the last minute to be a full dose for this round, which pissed me off but it was what Elango wanted and so here I go again… a human pin cushion.
I mentioned to the registrar about my breathing difficulties and he booked me into the thoracic clinic to get a lung capacity and function tests performed and they were completed on Friday the 28th, and I would be getting test results on the following Monday.
I didn’t get the results of my tests, so I still have no idea what the issue was, which frustrates me, because as this thing marches along and the year gets older, I seem to be kept in the dark more and more.
The aza cycle was not a lot of fun, and this time was actually worse, as it had been four months between cycles and my stomach has not healed as well as it did last time. On the 9th of September I was supposed to have my DLI, but once again it got screwed up because no-one had informed the day care nurses that it was going ahead and that really just finished me off as far as the hospital’s ability to organise anything. So once again, I had to go the next day too have the infusion. All went well this time and my body has responded a lot better than the last time, but my Hb still remains on the low side while all the other counts seem to be recovering well, so all the markers seem to be heading the right way. We shall see what new abuses are put on this body when I return to see my haematologist on the 21st.
In the meantime, I went to see one of the registrars, which is part of my weekly check-up and I have become more pissed off with this whole routine. I spend close to an hour on public transport, then an hour and some change after doing blood tests for me to spend five minutes in his office to tell me my blood results are similar to a week ago, and when I ask him what the plan is, he says he has no idea what is going on. I always leave more annoyed, as it is a waste of my time, and I know that I have plenty of time on my hands, but that coupled with what happened the week before with the failed DLI attempt and my finite patience is wearing extremely thin.
I also got a phone call from one of the transplant co-ordinators during the week to tell me that my next DLI is due on the 7th of October, so I, in typical sarcastic form, asked whether they were going to get this one right, as the last one had been a complete balls up. She said it wasn’t their fault that the last one had gone wrong, which annoyed me even more, so asked, well if it not your fault and it was definitely not mine, then who the hell stuffed it up. And the next one was the same shambolic mess as last time then I would be just going home and when they got their shit together then they could call me and I would see if I was available for the procedure to go ahead. That went down like a lead balloon, and she said I was to make myself available as the schedule was very tight. I reminded them that my time was also precious, and I had other appointments and that for the stuff up the week before I had cancelled two other appointments that I had on for the next day.
Hopefully, the message gets through that we also have other things to do as well.
Following the balls-up with the DLI, I had an appointment with Elango on the 21st of September, so I unloaded on him a bit about how I felt about all that had happened in the last month and how I felt like I was getting no information out of the registrar every time I came to the hospital. He understood where I was coming from and accepted that how I had been dealt with as far as the DLI and all that had followed since then was unacceptable and from now on all my appointments would be with him and not the registrars, so he gave me a deeper insight as to where all this was heading for the rest of the year, and that I was also about to start round seven of azacitidine, which I had suspected was going to happen anyway. At least this time it was a lower dose and so instead of it being two injections, it was now one… not so harsh on my stomach externally or internally as well. Yay, no nausea or anti-nausea medication.
With all this going on, my blood counts continue to be low and if my Hb drops any lower then I am going to end up having a transfusion again, but at least this time I will know the reasons why. All of this has also impacted on my physical health as well, as I am unable to play much golf, unless I use a cart and my bike is definitely unusable at the moment as I don’t have the energy at the moment for that either. In fact, the whole fatigue thing is really becoming quite chronic at the moment, and some days I struggle just to get out of bed and do what I have to get done… frustrating as all hell.
I completed my next DLi in early October and that went a hell of a lot smoother than the last one, but I got the feeling that the person who rang me up to book it in was unimpressed with what I said. I asked her in quite a surly tone, ‘is it going ahead this time on the day it’s supposed to, because if there was any delay, I was heading out the door and when they were ready to be a little bit more co-operative, then they could call me and I would check out my schedule to see whether I was available or not’.
She said it wasn’t her fault it was a cock-up on the last time, and that their schedules were very tight, and I had no right to threaten them. I carefully explained to her that my time was precious too and due to the last one’s mistakes, I had to cancel two other appointments and reschedule them to a later date because QLD health couldn’t get it together.
I also started the next round of aza on the 19th of October and again it was only a single injection , but this time I had some serious issues with my gut through the first four days of the course, not a nausea thing but just a general unwell feeling to the point that eating or drinking anything was quite difficult.
The good part coming out of all of this is that my blood counts are starting to recover even with the constant assault of chemicals and other things on my body. Elango seems pleased with the progress I’m making especially with the recovery of my platelets, but may Hb remains below 100, but that does not seem to bother him too much.
I was also at the time asked by my employer to fill out a work capability report, as to where I was in my treatment and the likelihood of my eventual return to work. The report came back stating that I would never return to work, based on my current progress, which I expected, but seeing it in writing puts an exclamation point on my continuing to work. He put down the worst-case scenario for me and on the 29/10/2020, I got a call from my employer. They said, based on what had been written in the report, they could not hold my job open for me anymore.
It feels like a kick in the guts, along with everything else I’ve had to endure this yea. This really is the final straw. Can’t wait for 2021 to come around. Hopefully it will be better than this shitty year.
Premature retirement and moving on
But that was not to be and so on the 6th of November 2020, I officially became retired after 43 years of being employed. The company I work for terminated my employment, as it was the only way I could keep my income protection going for another 12 months.
They had asked for a work capacity form to be completed by Elango, so they could ascertain what sort of work, if any, I was capable of performing now and in the distant future. He had put on the form, ‘will never work again’ and that my care was basically palliative care designed to enhance my chances of survival. And so my employer was left with no other option but to terminate me as there was no way they could hold my job any longer after such a blatant report was written.
It’s taken some time to accept that this is the correct decision as I do struggle quite badly with fatigue and the treatment has punished my body as well. I also doubt that I would ever get back to any sort of condition to return to work and be a functioning member of a workforce again and returning to shift work probably be impractical as well.
I harbour no ill will to either Elango or my former employer, as they are both only looking out for my best interests. I’ve been amazed by the amount of people I used to work with who were a bit pissed at the company’s decision to terminate me.
They thought bit was a bit callous given the COVID thing and the relapse, but once I explained to them that I was quite happy to go, and that it was a great relief to not only have the stress of the treatment but also trying to get back to work inside a timeframe off my back. It means now I only have to concentrate on getting better.

2021
As we start a new year, the treatments continue. On January 11th, I started my 11th cycle of azacitidine, with a lot more positivity than I ended 2020. I think I finished the year carrying a lot of anger, due to the year that I’d had, with the relapse, the battle with the income protection, and the many treatments and hospital visits had finally dragged me down.
But I think the thing that really topped it is off, was be forced into retirement. I think through 2020 both Karen and I had come to the conclusion I might not be able to work full-time, but to have it put so bluntly was an eye opener and I guess to come on top of everything else was the straw that finally broke the camel’s back.
I had an interesting conversation with Elango about everything that had transpired with the relapse, and how it was the most difficult conversation he ever has had to have, but he was amazed as to how well I had taken the news. I told him it was never easy hearing that sort of news, but I had to be pragmatic about my situation, so there was no point in me getting all upset.
So this year, I intend to approach my treatment with more positivity and I have accepted my retirement from work. On the 15th of January I went to my former place of work, as apparently they had a small farewell gift for me as a show of appreciation for all my hard effort through the years. Although it was rather low key, as I wanted, I think it put the final exclamation point to that chapter of my life and it helps me now to move forward with my life.
On February the 8th I will start my next cycle of azacitidine and hopefully I will find out what my next treatments entail.
I went to my appointment with Elango on the 8th of Feb and got news that my Hb had dropped to 75 and once again I was going to have a transfusion, for the second month in a row. I asked him if there was trouble with my bone marrow as I feel like I am going backwards. He said there were blast cells in my last blood test and, as such, he was going to do a bone marrow biopsy to get some answers and to also to set in motion an application for a different drug to control my condition. He feels we may be losing some control over my MDS with azacitidine. So at the moment it is a bit of nervous time.
Mind you I had a feeling that things weren’t quite right with my blood counts as I had issues with fatigue, I had two temperature spikes, one was 39.9, and I had to call an ambulance, but they got hold Elango and he said that if my temperature dropped to 38.5 and my heart rate stayed below 100 bpm, then I would not need to go to the ED.
At the same time I was also on a drug called Lyrica, which I was given for the nerve pain in my hands and feet and although it all worked fine, and the side effects were not severe, they were noticeable, in increased fatigue, headaches and constipation.
So at the moment I don’t know where my future treatment is heading or even what my future holds, which is rather scary.
On the 17th of Feb I had bone marrow number 11, to find out why, all of a sudden, my blood counts are dropping. In the last two weeks I have had two blood transfusions, one on the 10th as my Hb was at 75 and my platelets were also down to 160, and Elango seems to think that the azacitidine is now not controlling my MDS like it has and that we have to try a drug called venetoclax, which is just another form of control, but in a pill form, not a needle.
The amazing part of having such a low Hb, is that it does not feel like it is that low, except for some minor breathing issues. I’ve been able to carry on doing my normal things without a lot of difficulty. God help me if my blood counts return to normal, I won’t know what to do with all the extra energy I will have.
Anyway, I said to both him and the registrar that I was becoming just a little scared as stuff is happening, and it’s happening in the opposite direction to where I thought I should be heading.
It could just be like last year, where the treatment has worked too well and is suppressing my bone marrow from producing enough blood cells and there’s no point in speculating until I get the test results on the 25th of Feb, then I will know exactly what is going on and what the next course of action will be.
Karen and I attended my appointment on the 25th and as I suspected, the news was not good, it appears that my disease management through azacitidine was not working properly anymore and the progression of blast cells in my bone marrow was now at 22%, and so a new course of action is now required. I will be starting on March the 1st a drug called venetoclax, which is a pill, in tandem with cytarabine, a drug used in my initial induction chemo, which will hopefully control the issue, but I get the feeling, that this is the last roll of the dice for me.
Elango also said it appears there is something deeper going on, and in my original diagnosis 3½ years ago, I had a p53 deletion, which is the chromosome on the DNA strand that helps combat cancer in the body. He said that this p53 may also be corrupted and so all the issues I’m having may be tied to this corruption of that chromosome. He said under normal circumstances I would not have been recommended for transplant in the first place as the success rate is considerably lower, as is now being seen in what has transpired in the last 15 months.
At least on the financial front, it appears that I can do a TPD claim and still go for a Centrelink payment at the same time, as it appears the lump sum payment cannot be means tested as it comes from my superannuation. So we will make a TPD claim shortly and hopefully pay down all the bad debt that we still have, so that by the time the end of year comes around, all we have left in debt is our mortgage and we can go into next year in a better financial position than we have been in for years.
Venetoclax treatment
Also, on March 1st, I will be admitted into hospital for five days, as I start the new drug regimen then and so they want to monitor me for five days to ensure that I have no adverse reaction to the drugs.
It was decided on the 26th of Feb that I would not be admitted to hospital, as the original plan was, because my blood counts were reasonable, and so on March the 1st I had another appointment with Elango, and this time I dragged Karen along with me so she could again hear what was going to happen. It appears it was a bit of trial to see how a patient gets on without hospitalisation on this drug.
I was given a script for the venetoclax and instructions on how to start them, as apparently you cannot just start on a full dose as it can be rather dangerous. I was also informed that instead of them using cytarabine in conjunction with the pills it would be azacitidine instead. Apparently, my blasts were at 22% so they could not legally use cytarabine.
I was also given another blood slip and told to return on Wednesday to see how things were progressing. Karen and I dropped of the script at the pharmacy at 11.30am and were told it would be about an hour, so we said that was fine as we were going to have lunch, so the delay did not matter. When we got back to the pharmacy at about 12.45pm, we were told there was a delay in getting my script ready as they had to consult the doctor on a couple of things and so it went for the next hour or so, one bullshit excuse after another as to why there was a delay in my script being issued and the longer it took the more pissed off we were getting.
Considering that all the authorisations had already been done prior to us getting there, there should not have been any delay. Anyway, in the end I got the pills and another drug called allopurinol which is taken at the same time as the venetoclax, and away we went home. I started the pills on the 2nd of March and to date have had no major side effects from it. I eventually found out the true cost of this drug and it is $12,500 per month, but I get it on compassionate grounds, as normal chemo has failed to control my disease, so it costs me $28 a month.
On the 8th of March I started my next round of azacitidine and on the 9th, once again, I had another blood transfusion as my Hb had dropped to 85 again. When I spoke to Elango on the 8th, he told me to expect my blood counts to drop off over the next couple of months, as this is all part of the new treatment. I decided that this time I would just do the straight seven days instead of the five days with the weekend off and then going back on the Monday and Tuesday of the following week to finish of my cycle. Not too sure yet if that was a good idea, I’ll see how I feel the following week.
I still have to return to the hospital on the 15th for another review of how everything is travelling with treatment, etc, and judging by how my stomach feels and looks, not too good at the moment.
The review on the 15th went better than expected as it showed my blood counts were on the rise again, even my Hb, which has traditionally been slow in coming up, was back up over 100. I realise that I had a blood transfusion on the previous Tuesday, but the effects of those are usually only temporary, and since I was also have azacitidine injections at the same time, this was not a result I saw coming. Also, the other key indicator, which is my platelets were back up to almost 200, whereas last week they had been at just over 100. It seems that a combination of the azacitidine and the venetoclax is starting to work. I remain optimistic that going forward there is going to be continued improvement, now the only thing I need to get under control is my weight.
Since November 2020 I have lost almost seven kilos weight, which some would say, that’s great, but when you are not trying to lose weight but keep it on, then this much weight loss is quite disturbing. I prefer to be just that little bit overweight and going from 90 kilos which I was comfortable at down to 83 is a huge drop. I have been working with a dietitian at the hospital to try and get me onto a diet that hopefully gets some of the lost weight back on.
On the 29th of March I had another review on my blood counts which painted a much different picture, my Hb was down to 69, requiring yet another two bags of blood. I was officially neutropenic and my platelets were down to 55. The registrar said that they were happy with those counts as they are supposed to crash before they can recover. This is the nature of my treatment, but it is a bit depressing.
Although they may be happy with the way things are going and happy to transfuse when needed, it’s not very nice being tired all the time, hardly having the energy to start a small job but being unable to finish it because you lack the energy to do so. At the moment I am also getting tired of fighting this disease and all that it entails. But I continue to fight as I know no other way and it’s unfair on Karen who has put so much effort into this too, for me to just give up when things get a little tougher.
I start my next aza cycle on the 6th of April and due to Easter it will continue into the following weeks by one day. They wanted me to do a registrar’s appointment on that day too but I told them that wasn’t happening as my wife’s birthday was the day before and I had other things planned for the week that did not include extended hospital appointments. Luckily, they agreed, and we moved on from there.
Being neutropenic means my white cell count is low and so it was only a matter of time before I developed an infection and sure as eggs on the Thursday before Good Friday I got a small infection on my leg and so I am currently on antibiotics to try and solve that little charmer on my leg. Another pill to take on an empty stomach, so at the moment I spend six hours a day not being able to eat because of medication… and I wonder why I can’t put weight on.
I had my registrar change my antibiotic to something else that I could take with food, and so we sailed along fine.
I started my next round of aza on the 6th of April and that was a long day at the hospital as I got my registrar appointment all wrong and I was there an hour earlier than I needed to be, which pissed me off, so what I thought was a 12.40pm appointment, was actually 1.40pm and I finally got to see her at 2.30pm, which then meant I didn’t get my aza until 3.20pm. I was also told I’d be doing a blood transfusion the next day, which came as no surprise. Although all may other counts are doing ok, my Hb remains low, so I get transfusions as I need them.
So I rocked up for my normal aza injection at 9am only to be told my transfusion was being done down at radiation, which didn’t bother me until it came time to do the bags, which normally are done over 1-1.25 hours, but the orders said to do it over two hours, so what should have a 2½ hour thing for two bags took over 4½ hours and so by the time I got home at 5pm, I was tired, hungry and extremely pissed off.
The next day didn’t fare much better, there I was hoping I would be in and out inside an hour and home by lunch time. Never happened, because when they checked my temperature I was sitting at 38 degrees which sent the nurses into a panic as I should never be that high. But when I told them I’d been sitting in the mid-37s for weeks, they said I should have said something. They ran blood test and cultures and came to the conclusion that it was a combination of my disease and the pills on causing havoc in my body.
On the way out I ran into Elango, who I hadn’t seen for a couple of months, so I gave him a quick rundown on everything and he said it was probably the pills and not to get too concerned about it. At the same time, he gave me his doctor’s report for my TPD claim and off he went.
When I got a chance, I thought I would have a quick glance at what he had put down and in the conclusion for my prognosis, I have been given less than 12 months. I had to sit and read it twice just to make sure I wasn’t reading it wrong.
I always knew I only had short time left, at least 18 months to two years, but less than 12 months blew me away. When I showed Karen she was equally stunned, and said what are we going to do and I said, we get up each morning and do the exact same thing as yesterday. In other words we just carry on our life as normally as we have since this things started in 2017.
So the phone calls to let everyone began, and its not been pretty, but I keep saying nothing can undo this and we just need to stay strapped in for the ride. Some were disappointed that we would not be returning to NZ as we had hoped, but I’m not sure whether I can fly and, given the fact I’ve spent so much time at the hospital recently, I can’t see much changing for me from that point of view. Also, this being such an unpredictable disease and the treatment seems to be working, currently, then I may have a little longer or shorter, who knows.
Hospital stays
On April 19th I went in for a blood transfusion as per my appointment. Got hitched up and then they started the first bag. Within 15 mins I had spiked a temperature of 38.3 and so they stopped the transfusion and waited for the doctor’s advice as to what to do next. It took them over an hour to decide to do a chest x-ray to see if there was anything wrong as well as run some cultures from my blood to see if I had something running around in my blood that shouldn’t be there.
It was decided that whilst we wait, to discard the first bag of blood as the transfusion had been stopped for too long. So, in the bin the blood went. In that time the chest x-ray results had returned and showed a shadow on my lung that hadn’t been there in my previous x-ray about two weeks before. The suggestion was that it was fungal infection and they would start me on a treatment for that ASAP. The other thing the doctors decided was to start the second bag of blood, and so away we went with bag two.
Before the blood had even reached the pump, my temperature spiked again, so again the transfusion was stopped, this time for 20 mins whilst again the doctor was consulted. They decided to continue even though my temperature was high. In this time the doctor came back to see me and said I would need to have a CT scan of my chest to determine that it was a fungal infection and also have a bronchoscopy to see what sort of fungus it was, and would I do it as an outpatient? I just sat there and said I have had on bag of blood today and if they thought I was going to do this as an outpatient they could think again. I would rather stay in hospital until it was resolved properly, to which I think they were pleased and so was Karen, who is not trained to deal with this sort of thing.
So I was admitted to a ward called Epic, which I found out later is a short-term stay ward, and started on a course of intravenous antibiotics and an anti-fungal called voriconazole, also done as an intravenous drug, and so I settled in for the long haul.
The next day I was visited by one of the haematology doctors to explain the plan. I was to have a CT scan sometime during the day and I was also to have two more bags of blood, then they would arrange for the bronchoscopy to be done. Sounded like a good plan to me, so I was quite happy, until CT stuffed up and lost me their system. But the blood transfusions went ahead without a hitch and so I finally got the top up I needed. I finally ended having my CT down at the ED at 6pm so all was set. The people from thoracic came to explain about the bronchoscopy and what it entailed and it was decided it would be performed on the Friday as it was only a minor procedure with a twilight sedation involved. Nothing I hadn’t had before. So, on the Wednesday, I was finally discharged and sent home and I was more than happy to get back there as it had been a tough three days in hospital with bed changes and ward changes at 9pm, just to piss me off some more.
Thursday we spent catching on some of things we wanted to get done and it was a thoroughly enjoyable day just cruising and relaxing.
On the Friday I rocked up to my usual ward so they could give me platelets before the bronchoscopy. That all done, I went to thoracic to have my procedure, which was once again explained to me and in quick time I was in, sedated, and done. Apparently, whilst they were doing the scope, they found something else so they decided to do a biopsy at the same time. That’s when the fun started.
I awoke about an hour later, all fine, and they explained to me what they had done and why, gave me sandwich a coffee and a sheet on what I should look out for over the next 24-48 hours. So off I went home again, but being hungry, I suggested to Karen that we stop at a nice cafe and have something more substantial to eat than a sandwich. I ordered a nice pasta and that’s when it all started. I started coughing as I was having lunch and started to cough up small quantities of blood and the worse I coughed, the more blood came. Luckily there was a vacant block and I went down there to cough up the blood which was coming.
In the end I managed to eat sufficiently of my lunch and Karen picked me up at the vacant block where again I had had another coughing fit and went home. I had a quick shower and then lay on the bed wondering, what the hell I’d done to deserve this, and the coughing fits just kept coming and so did the blood, and eventually my lunch. In the end, I called an ambulance as this could not go on and the best place for me was back at hospital, so off to Ipswich ED I went, and the paramedics who were marvellous said there could be a bit of wait as we were being ramped, but then when they found out I was neutropenic, I was moved to a bed pretty swiftly as I’m a high-risk patient.
When the doctors at Ipswich learned what sort of patient they had on their hands, they were unsure how to treat me and so there were frantic calls to the RBWH haematology dept to see how to treat me. It was agreed to give me a bag of platelets, then give me intravenous antibiotic, take more blood cultures and blood tests, etc. It was also decided I could not return home whilst this was going on even though the blood had now slowed to an almost stop, but I couldn’t stay at Ipswich either as I needed more expert care than they could offer, so at 1pm I was sent the Royal and again the paramedics said it could be a long wait and I said to them, wait and see what happens when they learn I’m neutropenic, and sure enough within 10 mins I was in a bed out of harm’s way. Again, I had more blood tests and then I was moved up to ward at about 3am and so I was wrapped up warm and went to sleep.
Karen came up on the Saturday to bring me fresh clothes, toiletries, and my book, etc. She arrived just as the doctors were coming to see me, to see what was going on and to say what the plan was. So she got first what the drama was, and it appears they may have done something in the lung when they did the biopsy and so with the constant coughing, it wasn’t healing as the clots kept being taken out. So they put me on a pill to induce clotting in my blood since my platelets weren’t able to do that sufficiently. They put me an intravenous voriconazole and decided another CT would be done. A good plan.
All day I bought up no more blood and so I thought good we are starting to turn the corner, until in the evening some friends of the woman in the next bed bought in fresh flowers, and with their arrival I was coughing up blood again as I believe the spores or pollen had got in the air and triggered a coughing response. So here we go again, back to square one. I put a mask on and finally got to sleep and waited. On the Sunday Karen showed up just as the doctors were coming to see me about how I was going, and showed a little disappointment with what had happened the night before, but were still happy with my progress, carried on with drugs and arranged for the CT. I spent the rest of the day reading and sleeping waiting for my CT, which eventually got done in the ED again, but this time it was 11pm. Not happy.
Still on Monday, after some successful blood tests, I was finally discharged. After spending all ANZAC weekend in hospital, I was glad to go home. But not for long unfortunately. On the 4th of May after three days of spiking temperatures every day, I suspected that I might have an infection in my body. I made an appointment to see my GP to see if I could get some antibiotics and her advice to me was to go straight to hospital as this was out her league, due to the complexity of my illness. So Karen and I packed a bag, called an ambulance, and off to hospital I headed, again.
I was once again quickly admitted to the ED and once again if you mention I’m neutropenic, I get fast tracked in. So I arrived in a bay at ED at 5.30pm and was subjected to all the usual blood tests and cultures taken according to the wishes of the BMT team who are in charge of my treatment at all times and then left to await results. In the meantime, I was given a sandwich and a cup of coffee and left to wait form there. After about two hours it was decided to move me to a short stay area called cold, and it did live up to its name as it was freezing in the area and there I was left to await the decision as to what was going to happen to me and which ward I was going to end up in. So I spent an uncomfortable night on a hospital gurney trying to not only sleep but also keep warm. Oh and setting of the alarm on my pump as the doctor who put in the cannula had put it in the crook of my elbow and so when I bent my alarm whilst asleep it set the alarm off. Oh, that was a lot of fun… not.
In the morning, I was offered a breakfast of Weetbix and a cup of coffee and, left to my own devices, virtually saw no one for a couple hours unless I buzzed for something. At about 11am I was starting to get the shits on as no one from the BMT team had been to see me, so I went to the nurses station to see if they knew anything, because if not, I was going to remove my cannula and go home. All of sudden there was a flurry of phone calls to the BMT team and about 12pm I was told that someone from BMT would be down shortly to see me and sort things out. I didn’t hold my breath that they would rush down to see me, and I was right. It was 1.30pm that a registrar from BMT turned up to apologise for what had happened. It appears that no one other than me and Dr Butler knew I was in ED and they were sorting things out right then to move me up to ward and start me on antibiotics ASAP.
At about 4pm, I was finally moved to ward 7a north again and finally after over 22 hours on a hospital gurney I finally got into a hospital bed. Oh, the luxury, and finally I could have a shower and actually start to feel a little better. Never underestimate the power of a shower and a clean pair of clothes, and so I settled in ward life again.
It was decided that I was to be put into a single room as I was a droplet risk and the nurses weren’t sure what tests were going to be performed, so it was better to isolate me as a precaution. I thought, cool, at least I’ll get better sleep than being in a four-bed ward. So off I went and settled in for the next couple of days. Dr Butler came and saw me the next morning to explain that they were unsure whether the issue lay with me having an infection or whether it was a combination of the MDS and the fungal infection creating the issue. So I was placed on intravenous antibiotics to control any infection and we would see what happened from there. I was also told that my neutrophils had crashed below .10 and that was why they were taking such a cautious approach. I was also told I would be going on to GCSF injections to try and increase my white cell count. And so I was left to my own devices for the next couple of days and that they would look at discharging me on the Saturday if nothing major went wrong. It also appears that the fungal infection on my lung was shrinking, so it looks like the pills were working. Finally, some good news.
On the Friday I was ejected from my single room as it was needed for someone else, but it was actually good to be in a four-bed ward, although they are great single bed rooms, you do get quite lonely, so I moved again. I had blood tests and waited for the BMT team to give the results and what the plan was moving forward. But I never saw anybody until 9.30pm when once again a very red-faced registrar turned up apologising that once again I had been forgotten about, but she said that my chances of being discharged on Saturday were slim as my white cell count remained low.
How wrong she was, as Dr Butler came down on Saturday and said that could not find a source of infection and so they were putting it down to the disease and the fungal infection creating the havoc in my body, so there was no point in me staying in hospital and so I was to be given some antibiotics and GCSF injections to take home with me and I was to be back in clinic on Monday for review anyway, so I went home finally. I asked him what to do if I spiked a temperature at home, and he said unless it was not dangerously high to take to Panadol and let it settle down of its own accord and to figure out what triggers the spikes.
I quickly realised when I got home that it was having a shower that was creating the issue and the time of day that I have my shower, and so I have changed my routine to suit which is not a big deal.
Post-hospital stays
On the following Monday, I went back to hospital for blood tests and finally a catch up with Elango, who I had not seen since March, since I had started the ventoclax and so he told me that I would be staying on the anti-fungal medication for quite some time to ensure that it was beaten or my white cell count started to recover to the point that my own immune system could fight the infection itself. It also meant that I am not doing azacitidine until things return to normal. So there is a bonus to most things. I also had two bags of blood, but I was surprised when he told me that my Hb was 78 as it felt lower, but my white cell count was still shit.