You stepped up for Jack and his family in their darkest hour
Jack was 22 years old when he was diagnosed with a dangerous blood disorder called aplastic anaemia.
- Other blood cancers
- Treatments and side-effects

Jack was 22 years old when he was diagnosed with a dangerous blood disorder called aplastic anaemia.

Head of the Leukaemia Foundation’s National Research Program, Dr Peter Diamond discusses his role, priorities for the program, and exciting breakthroughs coming up in blood cancer research.

Gavin thought leukaemia was only a children’s cancer until the day his shock diagnosis completely changed his family forever.

After relapse last year, Siobhan knew her Leukaemia Foundation family would be there for her again.

Jenny connected with the vital information she needed to find her best treatment and take on her blood cancer with confidence.

Generous support helped deliver a research breakthrough that could lead to the first drug approved for patients with AL amyloidosis.

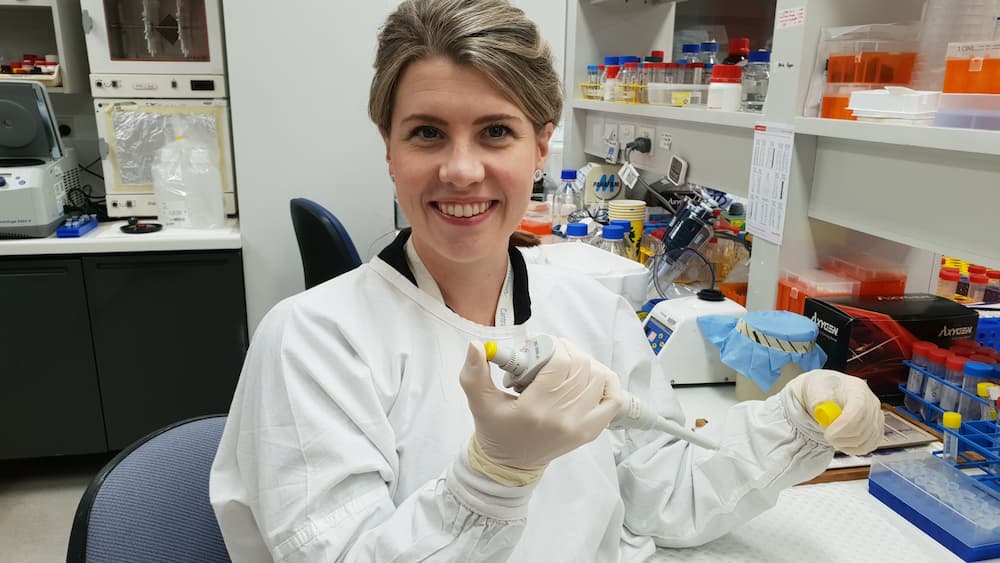
Dr Liesl Butler is just one of the promising young blood cancer researchers boosted by kind supporters.
After being diagnosed with an aggressive blood cancer, Sherma was left without access to the supportive care she need.

The Blood Cancer Taskforce has brought the Australian blood cancer community together to develop the first National Strategic Action Plan for Blood Cancer.
