Take charge of your cancer-related fatigue



Got questions?
We can help you make sense of it all
- Types of blood cancer
- Wellbeing during treatment
- Real stories
- Blood and bone marrow basics
- Blood cancer and COVID-19
Get support
We can support you through the roller coaster that is blood cancer
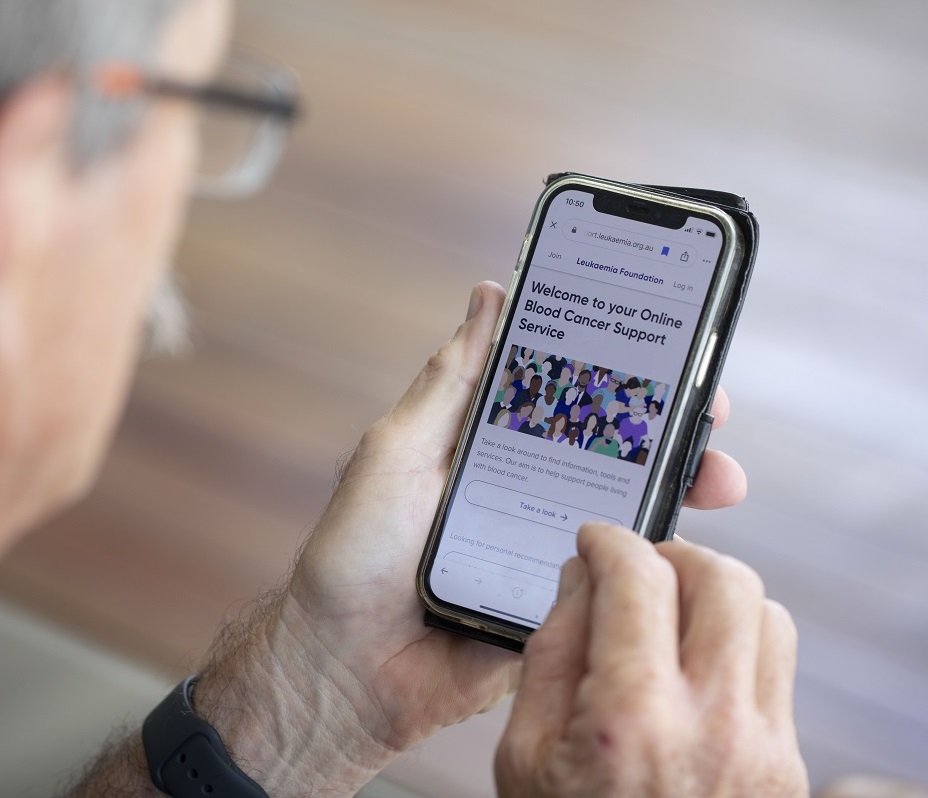
- Online Blood Cancer Support Service
- Accommodation during treatment
- Emotional support services
- Information and education services
- Support groups
Help save lives
Be part of the community that is conquering blood cancer
- Make a donation
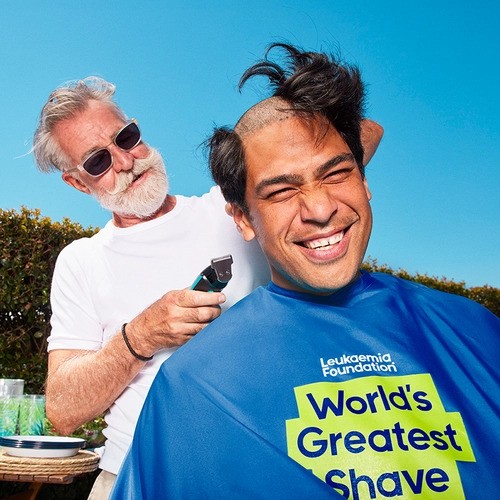
- Join an event or start your own
- Share your blood cancer experience
- Find out how your company can help
How you can show your support

Blood cancer information booklets for First Nations Australians

