Meet the Blood Cancer Taskforce: Carmel O’Kane
Taskforce member Carmel has been a cancer nurse for 24 years.
- Advocacy and policy

Taskforce member Carmel has been a cancer nurse for 24 years.

Meet Dr Rishi, a Consultant Paediatric Oncologist & Clinical Haematologist.

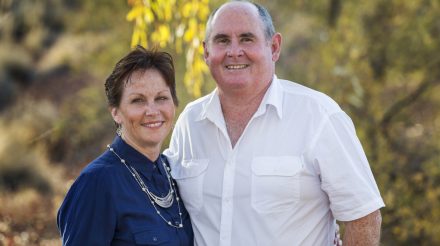
Not only do Lynette (Lyn) Healy and Lynnette (Lynnie) Coupar share the same name, but also the tragedy of losing a partner to blood cancer.
Dr Khai Li Chai is working to improve the prevention and treatment of infection in blood cancer patients with antibody replacement therapy.

Seven-year-old Neveah conquered a rare blood cancer after an international bone marrow donor search.

The Leukaemia Foundation has more than doubled the support of people living with blood cancer since COVID-19 hit Australian shores and is warning of more difficult times ahead.
Describing, understanding and improving the diagnosis of aplastic anaemia and bone marrow failure syndromes.

There’s an urgent need for new approaches to better prevent and treat GVHD.

Researchers such Dr Siok Tey are dedicated to driving rapid advancements in treatments, discovering new therapies, and launching innovative clinical trials.

The Nield family were overwhelmed by the care provided by the Leukaemia Foundation while their seven-year-old son Hodgkin lymphoma.
